-
PDF
- Split View
-
Views
-
Cite
Cite
David W Maidment, Margaret I Wallhagen, Kathryn Dowd, Paul Mick, Erin Piker, Christopher Spankovich, Emily Urry, New horizons in holistic, person-centred health promotion for hearing healthcare, Age and Ageing, Volume 52, Issue 2, February 2023, afad020, https://doi.org/10.1093/ageing/afad020
Close - Share Icon Share
Abstract
Over the course of a lifetime, the risk of experiencing multiple chronic conditions (multimorbidity) increases, necessitating complex healthcare regimens. Healthcare that manages these requirements in an integrated way has been shown to be more effective than services that address specific diseases individually. One such chronic condition that often accompanies ageing is hearing loss and related symptoms, such as tinnitus. Hearing loss is not only highly prevalent in older adults but is also a leading cause of disability. Accumulating evidence demonstrates an interplay between auditory function and other aspects of health. For example, poorer cardiometabolic health profiles have been shown to increase the risk of hearing loss, which has been attributed to microvascular disruptions and neural degeneration. Additionally, hearing loss itself is associated with significantly increased odds of falling and is a potentially modifiable risk factor for cognitive decline and dementia. Such evidence warrants consideration of new possibilities—a new horizon—for hearing care to develop a holistic, person-centred approach that promotes the overall health and wellbeing of the individual, as well as for audiology to be part of an interdisciplinary healthcare service. To achieve this holistic goal, audiologists and other hearing healthcare professionals should be aware of the range of conditions associated with hearing loss and be ready to make health promoting recommendations and referrals to the appropriate health practitioners. Likewise, healthcare professionals not trained in audiology should be mindful of their patients’ hearing status, screening for hearing loss or referring them to a hearing specialist as required.
Key Points
Hearing loss is associated with a range of negative health conditions, including poorer cardiometabolic health profiles, increased odds of falling, and is a potentially modifiable risk factor for dementia.
Health promoting activities, such as individuals adopting healthier behaviours or societies developing public health interventions, may help promote positive hearing health and minimise the negative health impact of hearing loss and related co-morbidities.
Healthcare professionals need to be aware of the range of negative conditions associated with hearing loss.
Hearing healthcare professionals need to be part of an integrated, interprofessional team, ensuring that holistic and person-centred care is delivered to older adults.
Longer lives are one of society’s most remarkable collective achievements; they reflect advances in social and economic development, as well as in health [1]. However, with the passage of time, numerous underlying physiological changes occur and the incidence of major burdens of disability from losses in hearing, vision and mobility increases. There is also an increased risk of developing chronic (or non-communicable) diseases, including cardiovascular diseases, chronic respiratory disorders, cancers and dementia [2]. Older age is associated with an increased risk of experiencing several chronic conditions simultaneously (so called ‘multimorbidity’), as well as the emergence of complex health states known as geriatric syndromes, which include conditions such as frailty, delirium and falls [2]. Thus, it is perhaps unsurprising that healthcare that considers and manages the complex needs of older age in an integrated way has been shown to be more effective than services that simply address specific diseases individually [3].
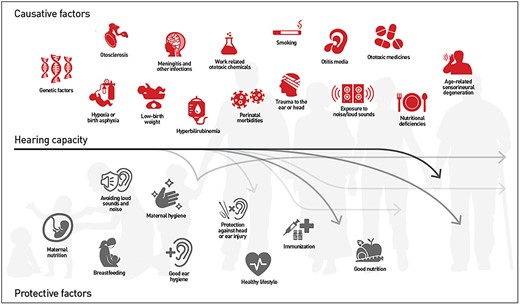
Globally, over 65% of people aged over 60 years experience some degree of hearing loss, with the prevalence of hearing loss increasing dramatically with age; hearing loss rises from 15% among people aged in their 60s, to >80% among those aged ≥80 years [4]. Hearing loss is a leading cause of disability; in 2019, the global number of years lived with disability attributable to hearing loss was 43.5 million [5]. Hearing loss impairs communication and social interactions [5], is associated with loneliness and social isolation [6], anxiety [7] and depression [8], as well as reduced quality of life [9]. However, the decline in hearing experienced in older age is not necessarily an inevitable degenerative process associated with growing old. Though some level of hearing change is inevitable with age (in particular, at high frequencies ≥8 kHz), the degree of loss is dependent on numerous modifiable and non-modifiable risk factors. Although not inclusive, the illustration in Figure 1 (source: [5]) highlights how both causative and preventive factors interact across a person’s lifespan to determine the occurrence, nature, severity, and progression of hearing loss [10]. As such, there are opportunities for intervention, in the form of prevention, identification, treatment and rehabilitation, across an individual’s life that could and should be addressed by healthcare practitioners. Subsequently, this publication will highlight our growing understanding of the range of health conditions that are associated with hearing loss and discuss potential health promoting activities that may help minimise the negative health impact of hearing loss and related co-morbidities. In addition, it will discuss how this evidence presents a new horizon for interprofessional teams to provide holistic and patient-centred hearing healthcare.
Risk and protective factors influencing hearing capacity across the life span. Source: World Report on Hearing; © World Health Organization 2021; Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo).
Associations between hearing and health
Hearing loss and physical function
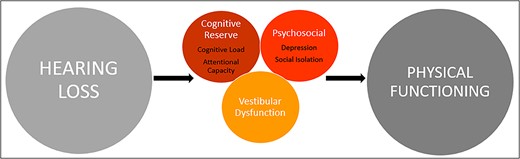
Decreased hearing acuity, like declines in other sensory systems, is multifactorial in nature. An accumulating body of evidence demonstrates the interplay between auditory function and other aspects of health. For example, epidemiological evidence demonstrates that hearing loss in older adults is independently associated with declines in physical functioning [11–13]. Maintaining optimal physical functioning is essential to healthy ageing, with declines leading to poorer quality of life and greater dependence, as well as increasing the risk of morbidity and mortality [14]. In addition to general declines in physical functioning, hearing loss in older adults is also a specific risk factor for falls [15]. Several mechanistic pathways underpinning the association between hearing loss and physical functioning have been postulated (Figure 2) and are discussed in detail elsewhere [16, 17]. Briefly, the cognitive reserve hypothesis suggests that, due to the requirement to process degraded sound signals, hearing loss results in an increased load on cognitive and attentional resources, which are also necessary for physical functions such as postural control and balance. Alternatively, it has been suggested that psychosocial difficulties, namely, social isolation, loneliness and depression, commonly experienced by older adults with hearing loss, mediate associations between hearing loss and physical functioning, termed the social cascade hypothesis. A further mechanism involves the vestibular system, whereby measures of hearing loss may act as a proxy for a concomitant vestibular loss, which leads to greater imbalance and falls.
Schematic of possible mechanisms underlying the association between hearing loss and physical functioning. The model posits that the association may be explained by the cognitive reserve hypothesis, psychosocial difficulties experienced by older adults with hearing loss (social cascade hypothesis) and/or vestibular dysfunction occurring concomitantly with hearing loss.
Hearing loss, cognitive decline and dementia
In addition to physical function, it is becoming increasingly recognised that hearing loss is associated with cognitive decline and dementia. Evidence from several systematic reviews has shown that adults with hearing loss have a greater risk of developing dementia than those without hearing loss [18–22]. Additionally, in a global review of modifiable risk factors for dementia, it was found that hearing loss was the greatest potentially modifiable risk factor for dementia in mid-life [23]. The proposed mechanisms of association between hearing loss and dementia are similar to those already discussed in relation to hearing loss and physical functioning, namely, cognitive reserve and social cascade. A further explanation is common cause, whereby hearing loss and cognitive decline share a common underlying pathology, such as oxidative stress or chronic inflammation, but are not causally related [24–26].
Hearing loss and cardiovascular health
Hearing loss is also associated with various chronic conditions, including cardiovascular diseases and their risk factors (e.g. diabetes, hypertension, smoking) [27, 28]. These associations can likely be explained by pathological changes within the vasculature of the inner ear, given that the cochlea is very metabolically active and relies on robust circulation for optimal functioning. Indeed, hypertension, smoking, diabetes and dyslipidemia are all associated with lower capillary density, reduced angiogenesis, increased capillary basement membrane thickness, changes in capillary supporting cell (pericyte) concentrations, inflammation, accumulation of reactive oxygen molecules and/or downregulation of vasodilators such as nitrous oxide [29]. Such structural changes can impair molecular transport (e.g. of oxygen, ions, glucose, metabolites or proteins) across capillary walls. Inflammation and oxidative stress caused by cardiovascular risk factors may also directly damage cochlear cells or extracellular proteins [30]. The pathological changes caused by poor cardiometabolic health accumulate with age, may accelerate age-related hearing loss and cause comorbid disease in multiple organ systems.
Given that metabolic risk factors for cardiovascular diseases are modifiable, and because they are highly prevalent, public health or clinical interventions to better address them could potentially result in significant improvements in hearing health. One of the most strongly supported interventions is physical activity; it is well established that regular physical activity in older adults can benefit multiple physical and mental health outcomes, including improved all-cause mortality and reducing the incidence of noncommunicable diseases [31]. Therefore, according to the World Health Organization’s (WHO) [31] evidence-based guidelines, for older adults to achieve optimal health benefits, the minimal recommendation is 150 to 300 minutes of moderate intensity aerobic physical activity, or at least 75–150 minutes of vigorous intensity aerobic physical activity per week. Nevertheless, older adults with hearing loss do not meet these guidelines, with a recent analysis of data from the English Longitudinal Study of Ageing (ELSA) showing that physical activity declines more rapidly in older adults who report hearing loss compared to those that do not [32]. Hearing loss specific barriers to physical activity have also been identified, including mental fatigue, as well as fear of alienation and stigma [33]. Environmental modifications and social support may nevertheless facilitate physical activity in this population [33]. On this basis, there is a need to mitigate the decline in physical activity and ensure physical activity is accessible in older adults with hearing loss to support healthy ageing [32].
Although it should be recognised that the reported associations between cardiovascular risk factors and hearing loss are inconsistent in the literature, and may only account for a small amount of variance, improved cardiovascular health has the potential to improve overall well-being and possibly reduce the risk for further hearing loss progression [34]. Even if the effects of better cardiovascular health on hearing are small for an individual, the societal benefits could be large, as poor cardiovascular health is widely prevalent [35]. Moreover, there is little risk that interventions targeting cardiovascular disease would exacerbate hearing problems. As such, there have been increasing calls for hearing healthcare to take a more interdisciplinary and holistic approach, as well as to address the broader health needs of individuals with hearing loss to promote overall health and well-being [36, 37].
A new horizon: interprofessional, holistic and patient-centred hearing healthcare
In 2001, the USA-based Institute of Medicine (now the National Academies of Science, Engineering and Medicine) emphasised that, to address the gaps in care, healthcare practitioners and organisations should no longer operate in silos, which results in a lack of complete information about an individual’s complex health needs [38]. To bridge this disparity, it was deemed essential for clinicians and institutions to collaborate to ensure that care was coordinated. This type of coordination and sharing of information is the core of interprofessional practice, which aims to provide integrated and patient-centred care to older people. This practice has been further outlined by the WHO’s recent 2019 guidance for integrated care for older people (ICOPE) [39]. The ICOPE approach proposes that care for older people should be based on a multi-step process that involves the following: (i) an assessment of an individual’s needs, preferences, and goals, including the identification of declines in key intrinsic capacities (e.g. vision, hearing, cognition, psychological health, physical health); (ii) the development of personalised, patient-centred care plans that involve multiple interventions to manage conditions associated with losses in intrinsic capacity; and (iii) the engagement and coordination of multiple healthcare services that are all driven to a single goal of maintaining intrinsic capacity and can be delivered through primary- and community-based care.
Unfortunately, however, Wallhagen, Strawbridge and Tremblay [36] have highlighted that there are few examples of holistic and interprofessional care described in the literature, especially as related to hearing healthcare. This is because there are several barriers to implementing interprofessional care in this context, including the structure of healthcare services that can make interdisciplinary communication difficult, as well as financial, regulatory and legal constraints [36]. Yet, to address the range of health conditions associated with hearing loss, and to minimise its negative impact on health, hearing healthcare must be integrated into the larger healthcare system. Further, to provide truly holistic and patient-centred care, providers across the spectrum of healthcare settings must incorporate hearing healthcare into their practices and become aware of the importance of hearing to health. Although a model of patient-centred care is yet to be developed specifically for hearing healthcare, Grenness and colleagues [40] investigated the views of older adults with hearing loss in relation to their preferences during audiological rehabilitation. Critically, these authors found that patients expressed a preference for individualised care in relation to the patient-practitioner relationship, information provision, and decision making. More recently, it has been suggested that a patient-centred approach to hearing healthcare should also incorporate evaluations of patients’ general health and lifestyle so that more targeted support can be provided to reduce the potential burden of multiple chronic diseases that frequently co-occur with hearing loss [41]. Subsequently, novel strategies and examples that aim to promote interprofessional, holistic and patient-centred practices that incorporate hearing healthcare are described.
The integration of hearing loss in diabetes services
Some recommendations are beginning to incorporate consideration of the value of including hearing healthcare providers within interdisciplinary healthcare teams. For example, persons with diabetes require many different specialists to address the problems they experience, including endocrinology, podiatry, optometry, dentistry, and pharmacists. Based on this, the USA’s Centers for Disease Control (CDC) has highlighted the need to address hearing loss in their ‘Diabetes and Hearing Loss’ online resources [42]. These materials (e.g. Take Charge of Your Diabetes: Healthy Ears [43]) support the ways in which the incorporation of hearing healthcare should be considered by other professionals to prevent the negative sequalae associated with diabetes. The CDC, for instance, recommends a baseline hearing test and balance screening at the time of diabetes diagnosis, followed by annual hearing loss testing. Current efforts to raise awareness of the effects of diabetes on hearing and balance in the USA are focused on involving physicians and diabetes education specialists. One recommendation is to assign the task of taking an online hearing screening and completing a brief balance survey as one component of diabetes education classes. The diabetes education specialist can then discuss this information with the patient or as part of a group session, along with recommendations for an appropriate follow-up. Another effort in the USA is to include hearing and balance recommendations in the discharge recommendations of hospital’s electronic medical records to ensure that this is considered if patients are seen at subsequent medical emergencies, such as stroke, heart attack, out of control diabetes or trauma. Automating the medical necessity of a referral for each patient takes away the issues of not seeing the invisible handicaps of hearing loss and associated risk of falls or other comorbidities.
Although such holistic recommendations are currently uncommon, the focus on diabetes by the CDC provides an example of the way in which audiologists and other hearing healthcare providers might use such data in their practices. Thus, for instance, when a person is identified with hearing loss, questions about vision and a vision exam can suggest the need for modifications in an individual’s dependence on speechreading and the need to incorporate other cues for communication. Alternatively, if a person with diabetes is having balance problems and is at risk of falls, referral to audiology, physical therapy or podiatry, as well as to persons with expertise in balance exercises, and the evaluation of potential vestibular problems, may be necessary. Vision is also integrally connected to the risk of falls and may need further evaluation. Furthermore, given the potential for peripheral neuropathy secondary to diabetes or chemotherapy, evaluation by neurology might be helpful.
The integration of hearing loss in dementia services
Given that hearing loss is associated with cognitive decline and dementia, it may be increasingly important for hearing healthcare professionals to communicate with other practitioners who work with persons with dementia and other cognitive impairments to assure a person’s hearing acuity is considered in advance of doing any cognitive assessments. Currently, there is very little hearing screening, nor diagnosis and treatment of hearing loss in advance of cognitive services [44]. However, the incorporation of routine audiology screening in memory services may be beneficial. In support, in a tertiary referral memory service in Ireland, McDonough and colleagues [45] explored the experiences, tolerability and understanding of having a hearing assessment in patients with mild cognitive impairment as part of their memory assessment pathway. In this study, hearing assessment involved a full audiological history, otoscopy, tympanometry, and both pure tone and speech audiometry completed by a hearing specialist (i.e. audiologist). Overall, the majority (90%) of participants were found to have at least a mild hearing loss, were satisfied with their experience of having a hearing evaluation and felt that it was an important part of their memory assessment. On this basis, the integration of audiology assessments into memory services may be worthwhile, especially given the amount of hearing loss detected and the potential impact of hearing loss on future cognitive decline [45].
Practical considerations for increasing awareness of hearing loss in healthcare professionals
A further consideration is that healthcare practitioners in general need to be aware of hearing ability when providing counselling and discussing plans of care because miscommunication can occur and impact safe and effective care [46, 47]. In this regard, there is a need to educate multidisciplinary, primary healthcare teams (e.g. general practitioners, practice nurses, etc.) and other healthcare professionals about the importance of hearing to health, as well as about the need to implement valid screening tests for hearing capacity. This is essential because hearing loss is not easily recognised in a one-on-one, face-to-face meeting in a quiet examination room. Hearing loss is invisible and may not be identified if the person is only asked if they have a hearing loss. The issue of anosognosia, the inability of the patient to know they have a sensory impairment, as well as the stigma often associated with hearing loss and hearing aids, often limits the subjective recognition of hearing loss. Primary healthcare teams should also be mindful of other sensory losses, including visual acuity, given the prevalence of vision loss similarly increases with age. Moreover, while the prevalence of dual sensory (i.e. hearing and vision) loss in the USA may be less than 1% among persons under that age of 70, it rises to 11.3% among individuals 80 years and older [48]. Thus, the occurrence of visual impairment must also be considered when screening and testing hearing.
There is now a range of possible hearing screening tools available that could be easily incorporated into various primary healthcare settings. Commercially available and calibrated screening equipment (e.g. screening audiometer and otoacoustic emissions) that do not require a hearing specialist are an option. Alternatively, where screening or diagnostic audiometry is not available or would be inappropriate, screening applications (or apps) for smartphones or tablet computers may be a suitable alternative (e.g. ‘hearWHO’ [49]). Although these tests already exist and are available, they are not currently implemented in routine clinical practice [36]. Therefore, there is a potentially unexploited, yet viable, opportunity for primary healthcare teams to incorporate low-cost hearing tools into their practices. In doing so, this could facilitate a more patient-centred approach, whereby patient–practitioner interactions, information provision, and decisions about management and treatment options are tailored to the individual, empowering them to be a more active participant in their healthcare.
In addition to hearing tests, including questions about understanding speech in noise may help to uncover hearing difficulty [50]. Spankovich and Yerraguntal [51], for instance, recommended a series of questions for screening patients with diabetes for hearing loss, which can also be easily translated to other patients without diabetes by removing question 4:
Do you or your family perceive any change in your hearing?
Do you have hearing difficulty in quiet places or noisy places?
Have you had your hearing tested in the past 2 years?
Do you know how diabetes can affect your hearing?
Do you know what to do if you perceive a change in hearing?
Do you know how to reduce your risk for hearing loss?
If the patient answers ‘Yes’ to questions 1 or 2 or ‘No’ to questions 3–6, it is recommended they be referred for an audiological evaluation. Validated questionnaires such as the Hearing Handicap Inventory for Adults or Elderly [52] and Speech, Spatial and Qualities of Hearing Scale [53] have also been suggested as potentially suitable screening tools [54, 55]. Another strategy is to use a combination of questions with a finger-rub or whispered voice test [56], with referral for audiological evaluation for those who test positive on either or both assessments. Nevertheless, the whisper and finger-rub tests lack calibration, standardised application, and have low sensitivity to mild-to-moderate hearing losses [57]. In addition, studies have shown that some self-report questions may be more effective than others when assessing hearing loss. For example, when testing the validity of hearing loss questions, Gibson and colleagues [58] showed that the question, ‘Is your hearing (with or without a hearing appliance) – Excellent, Very Good, Good, Fair, or Poor?’, demonstrated the highest sensitivity and specificity when compared to the whispered voice test. In contrast, questions related to the ability to follow a conversation in the presence of others or use a telephone showed low sensitivity, with the latter deemed entirely ineffective.
It should also be noted that, regardless of the patient’s hearing status, healthcare professionals should make sure that consultations with older adults take place in a quiet room free of distractions, and should speak clearly and slowly, while ensuring that their face and lips are visible. In addition, incorporating a personal amplifier (e.g. ‘pocket talker’) in practice settings can facilitate communication with persons with hearing difficulties who do not use hearing aids. For those with hearing aids, it is essential to assure that the batteries are working, and that the device is switched on.
Concluding remarks
In summary, this article highlights why there is a need for interprofessional teams to provide holistic and patient-centred hearing healthcare. As a ground to this involvement, it is important for the (hearing) healthcare professional to be aware of the range of conditions associated with hearing loss and the way in which hearing loss places individuals at risk for other negative health effects, such as falls, dementia and poor cardiovascular health, as well as misunderstandings in the healthcare setting. These understandings, emphasised in the current publication, can also broaden holistic, patient-centred care provided in all hearing and general healthcare settings to support healthy ageing.
Declaration of Conflicts of Interest
Dr Emily Urry is a Senior Manager in Digital Health Innovation at Sonova AG, Switzerland.
Declaration of Sources of Funding
This work was supported by the brand Phonak, which is part of the Sonova Group. The funding arrangement specified that the sponsor had no right to sensor the article or preclude publication.
References
Hearing diffculty is associated with reduced physical activity: a 20-year cohort study from the English longitudinal study of ageing. https://www.baaudiology.org/conference/abstracts-posters-free-papers/ (14 February, last accessed).
Public Lecture: Improving Physical Activity in Older Adults with Hearing Loss. https://www.ncsem-em.org.uk/events/physical-activity-and-hearing-loss/ (14 February, last accessed).



Comments