Oral Manifestations of COVID-19: Updated Systematic Review With Meta-Analysis
- 1Department of Medicine and Medical Specialties, Faculty of Medicine and Health Sciences, University of Alcalá, Alcalá de Henares, Spain
- 2Department of Preclinical Dentistry, School of Biomedical Sciences, Universidad Europea de Madrid, Madrid, Spain
- 3Department of Clinical Dentistry, School of Biomedical Sciences, Universidad Europea de Madrid, Madrid, Spain
- 4Department of Dentistry, Federico Henriquez y Carvajal University, Santo Domingo, Dominican Republic
- 5Department of Surgery, Instituto de Investigación Biomédica de Salamanca (IBSAL), University of Salamanca, Salamanca, Spain
- 6Dean of the Faculty of Dentistry, Universidad Alfonso X El Sabio, Madrid, Spain
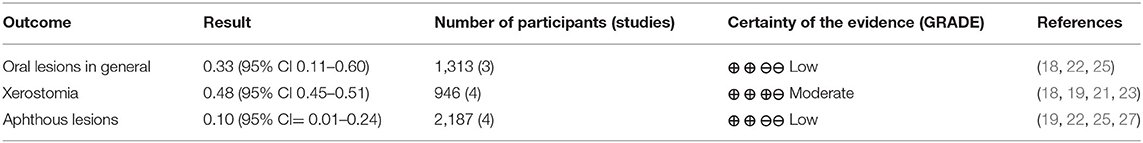
There is increasing evidence for oral lesions and manifestations of COVID-19. The aim of this meta-analysis was to investigate the types of oral manifestations of COVID-19 and their prevalence. PubMed/Medline, Scopus, Web of Science, and Google Scholar databases were used to search for publications on oral manifestations in patients with PCR-confirmed COVID-19. A total of 310 records were selected, and 74 were included. Oral lesions in COVID-19 were classified according to their etiologies, including iatrogenic lesions caused by intubation and opportunistic infections. Of the included studies, 35 reported oral lesions probably caused by severe acute respiratory syndrome-Coronavirus-2 (SARS-CoV-2) infection. Meta-analysis of prevalence data on oral manifestations and aphthous lesions indicated high heterogeneity, while meta-analysis of xerostomia prevalence data revealed a pooled prevalence, with considerable heterogeneity. In conclusion, the meta-analysis yielded high heterogeneity between studies: oral lesions yielded a prevalence of 0.33 (95% CI 0.11–0.60), xerostomia lesions a prevalence of 0.44 (95% CI 0.36–0.52) and aphthous lesions 0.10 (95% CI 0.01–0.24). In addition, a gap in the evidence regarding the prevalence of oral lesions in COVID-19 was identified and the need for further observational studies focusing on this issue and on the causal relationships between oral lesions and COVID-19 was highlighted.
Introduction
In a span of a few months, coronavirus disease 2019 (COVID-19) has developed into a full-scale global pandemic of epic proportions that affects all age groups with considerable mortality, various sequelae in survivors, and grave socio-economic impact on society (1, 2). Involvement of multiple body systems and organs, including the lung, gastrointestinal tract, liver. blood vessels, heart, nervous system, and kidneys, has been reported in patients with COVID-19 (1). The varied presentations of this disease are under intense study in the hope of better understanding its pathogenesis.
Numerous oral lesions have been reported in patients with COVID-19 (3–8). These manifestations include a wide and varied range, from the inflammation of the papillae of Wharton's duct to plaques on the tongue; however, the exact relationship between many of these lesions and pathologic processes of the severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) infection is still a subject of investigation (9). Some of these lesions can clearly be attributed to causes other than the direct effects of SARS-CoV-2 infection. Drug reactions and lesions caused by prolonged intubation are in this group. Moreover, given the sheer number of people afflicted with COVID-19, it is expected that some of the oral lesions seen in these patients are coincidental. Nonetheless, there is growing evidence that a substantial number of oral lesions in COVID-19 are directly related to the pathological processes of the disease (10).
Considering that systematic reviews are an essential tool for synthesizing available scientific information and identifying areas of uncertainty where research is crucial, the present systematic review and meta-analysis (SRMA) aimed to investigate the oral manifestations of COVID-19. A better understanding of the oral manifestations of COVID-19 could help elucidate the pathologic processes involved in this infection and prepare the physician, dentist and health care personnel to cope with the disease. Taste disturbance, which is generally described in conjunction with anosmia, is a prime symptom of COVID-19 (11). This symptom was not addressed in the present review as it clearly surpasses the confines of the oral cavity and involves the sense of smelling.
Materials and Methods
The present systematic review and meta-analysis (SRMA) follows the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement (12).
Eligibility Criteria
Methodological guidance from the Joanna Briggs Institute on the critical appraisal of prevalence studies and studies of etiology were followed in determining the eligibility criteria (13, 14), and participants, exposure, outcome, study design, as well as context, were taken into consideration. Inclusion criteria encompassed studies reporting oral lesions in patients with PCR-confirmed COVID-19 diagnosis. The primary outcome of interest was the prevalence of oral manifestations of COVID-19. Observational studies, including prevalence studies, case series, and case reports, were included in the review. As for the exclusion criteria, taste disturbances were not included in the review. In studies of mucocutaneous lesions in COVID-19, only cases with oral involvement were included. The eligibility criteria were determined through discussion and consensus among the authors.
Search Protocol
The eligibility criteria described above were used to design specific search strategies for databases. PubMed/Medline, Scopus, Web of Science, and Google Scholar databases were searched for published and in publication records from December 1, 2019, to March 10, 2021. No language restrictions were applied. The search strategies for these databases are given in the Supplementary Materials 1–4. Moreover, we manually searched the references of review articles on the subject to identify further relevant papers.
Study Selection
Duplicate records were removed from the collated search results, and titles and abstracts of the remaining records were screened. Records that did not meet the eligibility criteria were discarded. The full texts of the remaining articles were examined, and, again, those that failed to satisfy the eligibility criteria were excluded. Papers were selected in parallel, but independently, by JA, AS and JMA and the reviewers discussed discrepancies in the results and reached a consensus.
Data Collection
Relevant information on geographical location and design of the study and data on the prevalence of oral lesions and their subgroups were extracted from prevalence studies. In case reports and case series, information on geographical location and design of the study, participants' sex and age and general and oral signs and symptoms were extracted. Specific forms designed by the reviewers were used in data extraction.
Risk of Bias Assessment
The Joanna Briggs Institute's Critical Appraisal Checklists for Studies Reporting Prevalence Data was used to assess the risk of bias in prevalence studies. For assessing case reports and case series on lesions caused by SARS-CoV2 infection, the Joanna Briggs Institute's Critical Appraisal Checklist for Case Reports and Case series were used, respectively (15). The risk of bias in a study was considered high if the “yes” score was 49% or lower. Studies with a score between 50 and 69% were considered at moderate risk and those with a score of 70% or higher at low risk of bias. The reviewers could override the evaluation and modify the risk of bias by consensus, providing specific reasons.
Data Synthesis
The main outcome of interest was the prevalence of oral manifestations of COVID-19. Available data on the prevalence of oral lesions in general and their subgroups were synthesized, and a meta-analysis of prevalence was performed on them. Oral lesions in patients with COVID-19, reported in case reports and case series, were classified according to their putative etiologies, e.g.,: oral manifestations caused by SARS-CoV-2 infection, opportunistic co-infections, and iatrogenic lesions. For oral manifestations caused by SARS-CoV-2 infection, relevant data on patient and disease characteristics and oral manifestations were summarized in table form and qualitative synthesis was performed. Heterogeneity among the prevalence studies was computed using the Q statistic and the I2 index. The random effects model was used in the meta-analysis. The meta-analysis of prevalence was performed using the approach proposed by Barendregt et al. (16). Double arcsine transformation was employed to stabilize the variance, and overall prevalence (95% CI) was calculated. The leave-one-out sensitivity analysis was performed to explore whether the inclusion of the studies at high risk of bias in the meta-analysis distorted the results. Meta-analysis was performed using MetaLX (Version 5.3) software for meta-analysis in Microsoft Excel. The significance level was set at P < 0.05. Meta-regression analysis of the prevalence studies was performed with three moderator variables of the geographical location of the study, study design, and risk of bias. The MARegresData function in MetaXL was used to create regression datasets for studies on the prevalence of oral lesions in total, aphthous lesions, and xerostomia. The regression data set contained transformed effect sizes with standard error and variance, un-transformed effect sizes with lower and upper CIs, and normalized weight of studies. These data were transferred to STATA statistical software, version 16 and analyzed using the “Regress” command and robust (Huber-Eicker-White-sandwich) standard error estimation. P-values <0.05 were considered significant.
The Certainty of Evidence Assessment
The certainty of evidence in prevalence studies was assessed using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach (17). The evidence was rated according to the level of concern in the domains of the risk of bias, inconsistency, imprecision, indirectness, and publication bias. Publication bias was assessed by drawing funnel plots and visually inspecting them.
Results
Characteristics of the Studies
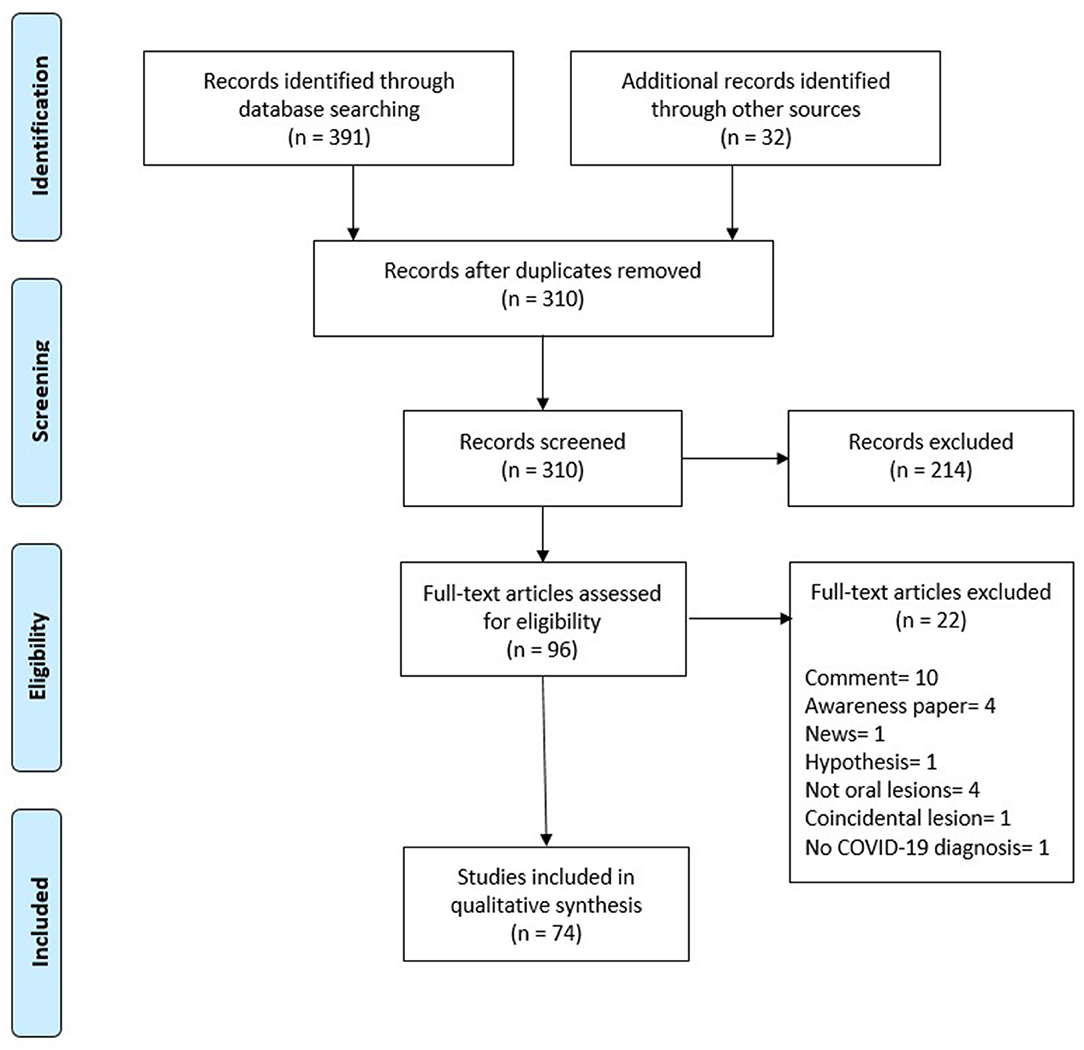
As of March 10, 2021, 391 records were identified. An additional 32 records were identified by searching references from relevant review articles. After removing duplicate records, 310 entries remained. The titles and abstracts of these records were studied, and 214 records were excluded at this stage. A total of 96 articles were searched for eligibility, excluding 22 studies at this stage because they either did not include reports of oral manifestations in patients with COVID-19 or reported coincidental oral lesions that were clearly not caused by COVID-19. One excluded article reported oral lesions in a patient with suspected COVID-19 without PCR confirmation of disease. Thus, 74 studies on oral manifestations in patients with COVID-19 were selected for review. Of these 74 records, 10 were prevalence studies and the remaining 64 were case reports and case series on oral manifestations (Figure 1, Flowchart).
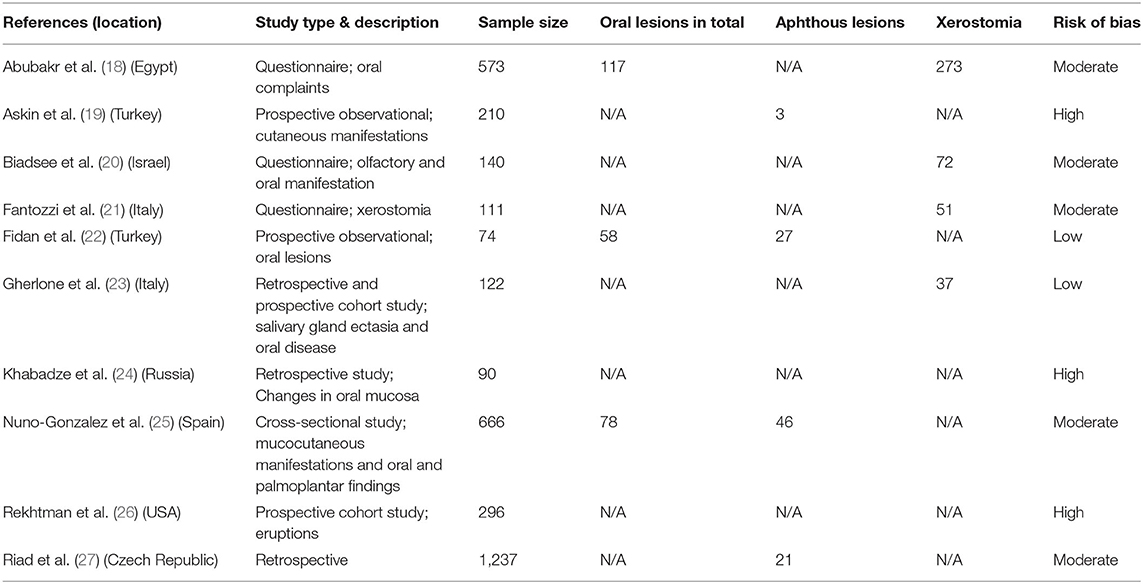
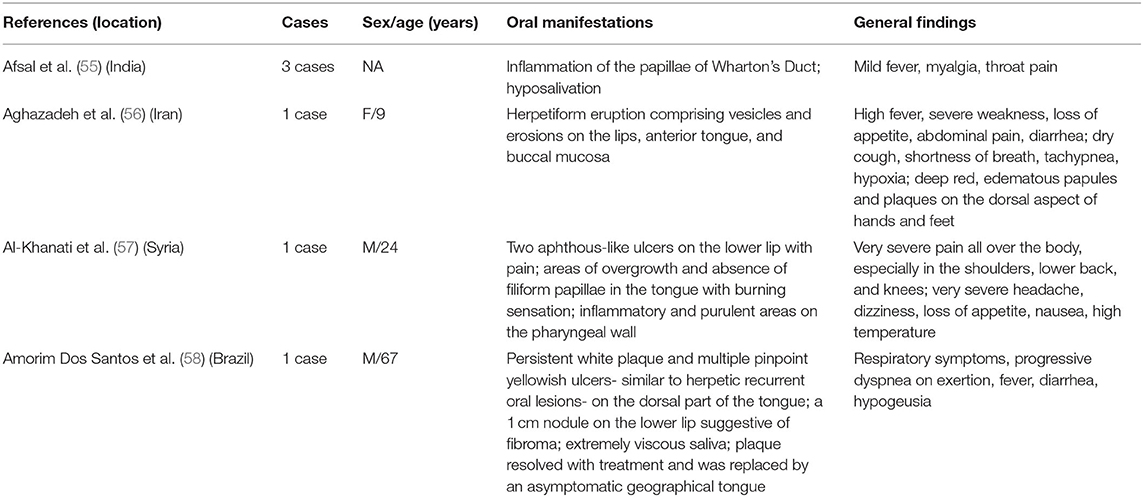
A total of 10 studies with information on the prevalence of oral manifestations in COVID-19 were identified (18–27), with a total of patients included in these studies was 3,519. Three reported the number of patients with oral lesions in general (18, 22, 25), four gave the number of patients with xerostomia (18, 20, 21, 23), and four mentioned the number of patients with aphthous lesions (19, 22, 25, 27). A total of 64 records retrieved were case reports and case series of oral manifestations in COVID-19. These cases were classified according to their presumed etiologies into three main categories and eight etiologic groups. In the category of oral manifestations with probable causes other than SARS-CoV-2 infection, iatrogenic lesions (lesions from intubation and other invasive procedures) (28, 29), drug reactions (30), and opportunistic co-infections with Candida albicans (31–34) or Herpes simplex (35–39) were included. The second category comprised multiorgan syndromes with variable oral manifestation. Clinical entities in this group usually involve several organ systems, but the oral manifestation in them is not constant and is observed in only a percentage of patients. Multisystem inflammatory syndrome and Kawasaki-like disease (40–53), as well as oral lesions that are part of other multiorgan involvement (urticaria and angioedema with mouth involvement) (54). he third group included oral manifestations caused directly by SARS-CoV-2 infection, such as relevant oral lesions (7, 55–85) and salivary gland involvement (86–89); 35 studies reported cases and case series with oral lesions in COVID-19 with no apparent non-COVID-19 causes. The characteristics of these studies are summarized in Tables 1–3.
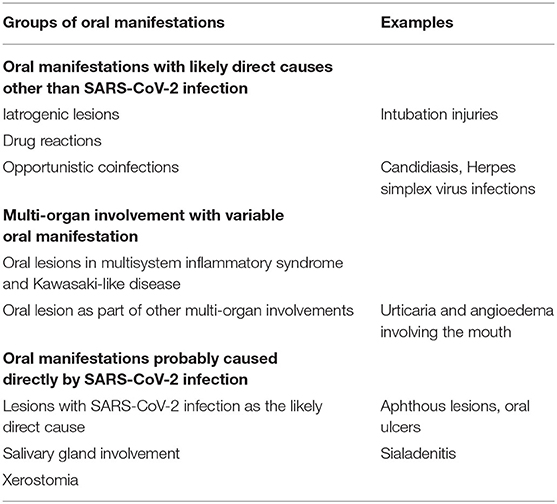
Table 2. Classification of oral manifestations (except taste alterations) in patients with COVID-19 according to etiology.
Risk of Bias Assessment
The risk of bias was assessed using Joanna Briggs Institute's Critical Appraisal Checklists for Studies Reporting Prevalence Data, and then, the reviewers examined and finalized the results of the assessment. Overall, 10 prevalence studies were assessed (18–27). In two study, the risk of bias was determined as low (22, 23), in five studies as moderate (18, 20, 25, 27), and in three as high (19, 24, 26). The risk of bias assessment and the reasons for the upgraded assessments are given in the Supplementary Material 5.
Results of Meta-Analysis
Table 1 shows 10 studies addressing the prevalence of oral lesions in COVID-19. Data on the prevalence of oral lesions in general, xerostomia, and aphthous lesions were meta-analyzed. For each of these three variables, studies reporting data on that variable were included in the relevant calculations. In groups that contained studies at high risk of bias, the meta-analysis was repeated after removing those studies. Of 10 studies, three reported data on more than one variable (18, 22, 25) and were accordingly included in more than one analysis; while two studies did not report data for any of the three variables (24, 26) and therefore, were not included in the calculations.
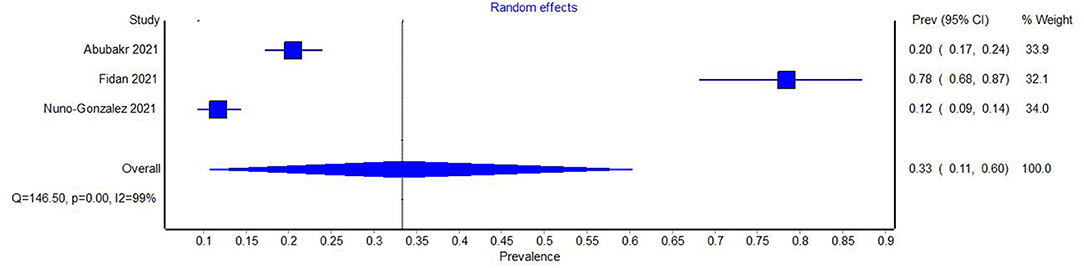
Among prevalence studies, three presented data on the number of patients with oral lesions in general (18, 22, 25). The heterogeneity of the studies was examined using Cochran's Q test and the I2 index. Both these measures indicated very large heterogeneity among the studies (Q = 146.50, p = 0.00, I2 = 99%). The Meta-analysis of the prevalence of oral lesions in general in COVID-19 yielded a prevalence of 0.33 (95% CI 0.11–0.60) (Figure 2). The sensitivity study did not lead to a significant difference in the results.
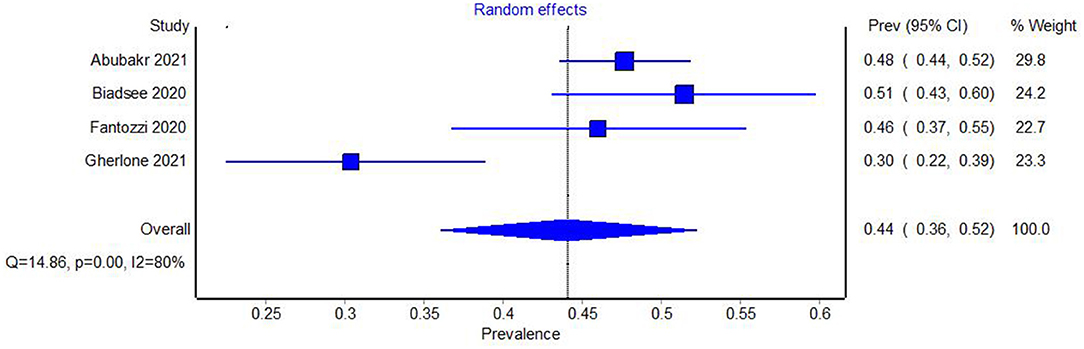
A total of four studies reported the number of patients with xerostomia in the sample under study (18, 20, 21, 23). Cochran's Q test and the I2 index were used to examine the heterogeneity of the studies, both of which revealed large heterogeneity among the studies (Q = 14.86, p = 0.00, I2 = 80%). The Meta-analysis of the prevalence of xerostomia in COVID-19 yielded a prevalence of 0.44 (95% CI 0.36–0.52) (Figure 3).
Among prevalence studies, three reported the number of patients with aphthous lesions (19, 22, 25), one of which had been evaluated as being at high risk of bias (19). The heterogeneity of the studies, including the one at the high risk of bias, was examined using Cochran's Q test and the I2 index. Both these measures indicated very large heterogeneity among the studies (Q = 98.77, p = 0.00, I2 = 97%). The Meta-analysis yielded a prevalence of 0.07 (95% CI 0.01–0.16) (Figure 4).
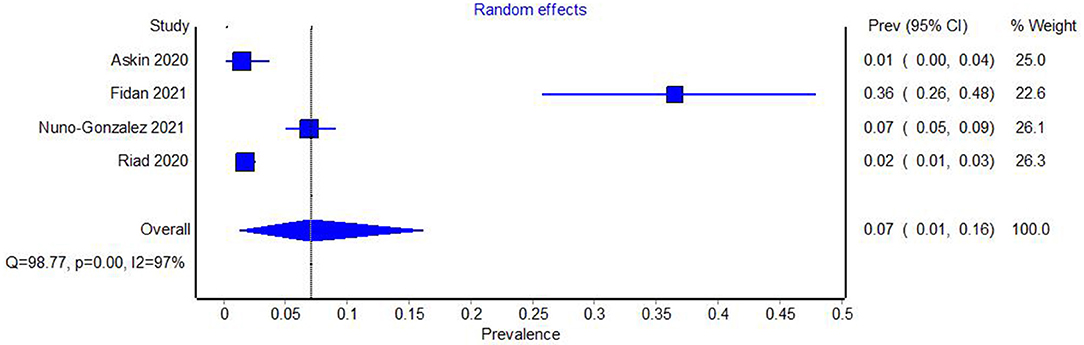
Figure 4. Forest plot showing the pooled prevalence of aphthous oral lesions in COVID-19, with studies at high risk of bias included.
The study with a high risk of bias was eliminated from the analysis and the heterogeneity tests and meta-analysis were repeated. Again, high heterogeneity between studies was evident (Q = 95.22, p = 0.00. I2 = 98%). The prevalence of aphthous lesions in COVID-19 was 0.10 (95% CI = 0.01–0.24) (Figure 5).
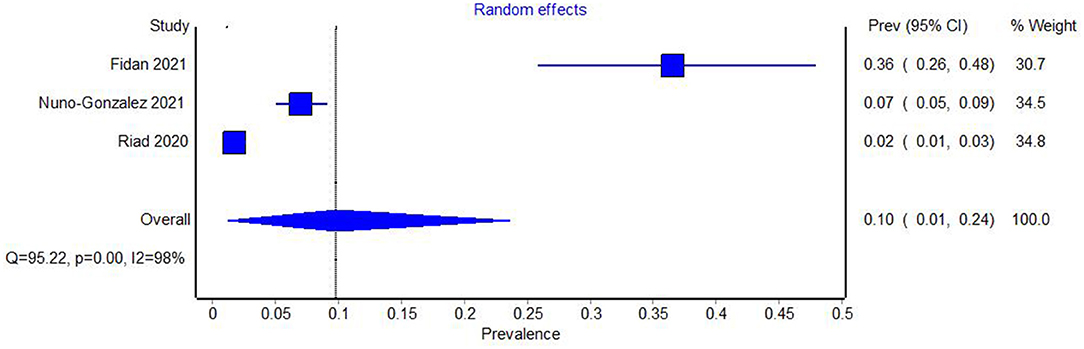
Figure 5. Forest plot showing the pooled prevalence of aphthous oral lesions in COVID-19 with studies at high risk of bias excluded.
In the meta-regression analysis of prevalence studies, three putative moderating variables were studied: geographical location of the study, study design, and risk of bias. No significant relationship was detected between these variables and the prevalence estimate for oral lesions in total or the prevalence estimate for aphthous lesions. In xerostomia studies, variables of study design and risk of bias showed an effect on the prevalence estimate (R-squared = 0.9417, p < 0.003).
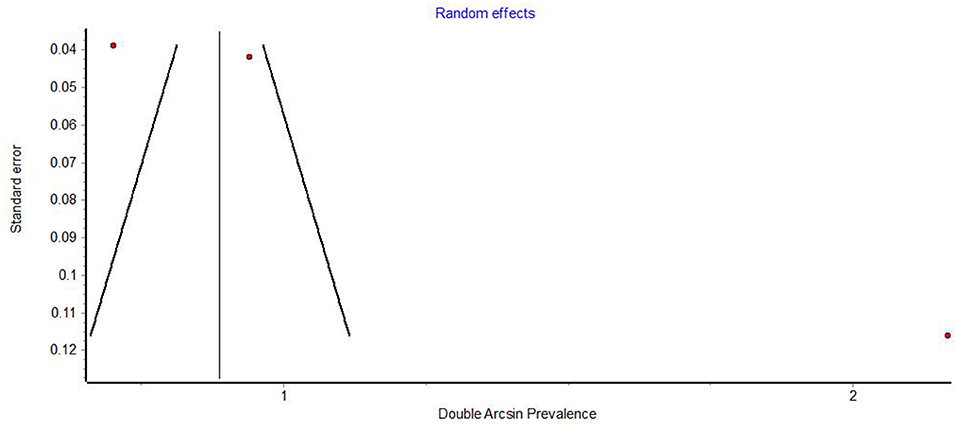
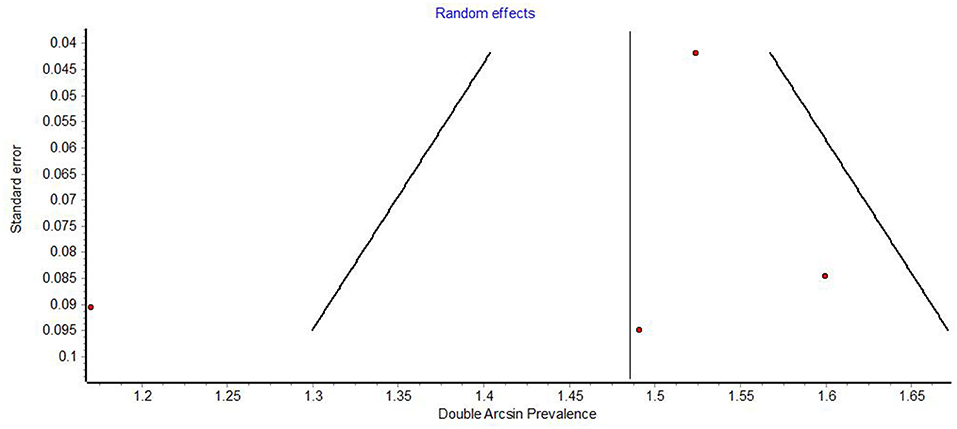
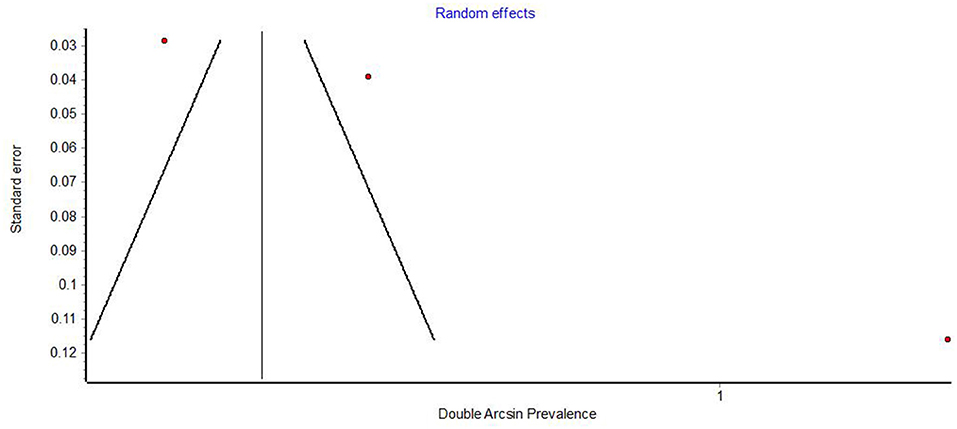
Funnel plots demonstrated obvious asymmetry, indicating the presence of high publication bias (Figures 6–8).
The GRADE tool assessed the prevalence of oral lesions in general and aphthous lesions as low, while the prevalence of xerostomia was assessed as moderate (Table 4).
Discussion
To date, very few studies have been published that directly address the question of the prevalence of oral manifestations in patients with COVID-19 using adequate detection methods. Much of the data available on the subject is still evidence from studies on mucocutaneous involvement or data gathered through patient questionnaires. Nonetheless, the SRMA of prevalence data on oral manifestations in COVID-19 at this stage, can identify and define important gaps in evidence and set the stage for further research, and even provide preliminary results of great interest.
The number of studies reporting on the prevalence of oral manifestations in COVID-19 remains very low and the problems mentioned above, make the existing reports at considerable risk of bias. A comprehensive search of the relevant literature identified only 10 primary studies with data on the topic (18–27), with the risk of bias being high in three studies, moderate in four and low in two. Three studies relied on patient-directed questionnaires as the data collection vehicle (18, 20, 21), a fact that is bound to impact the accuracy of the data. In addition, many of the studies did not focus on oral lesions but mentioned these lesions within the framework of a broader study on mucocutaneous lesions. Similarly, some of the prevalence studies focused on a specific type of lesions, e.g., xerostomia or rashes (21, 26), despite the reviewers improved the risk of bias assessed for some of the included studies (19, 23, 24, 26).
On the other hand, the included studies report on the prevalence of oral manifestations of COVID-19 in three categories: oral manifestations in general, xerostomia, and aphthous lesions. In the studies concerning the prevalence of oral lesions in general and aphthous lesions, tests showed a very high degree of heterogeneity- I2 = 99% for oral lesions in general and I2 = 98% for aphthous lesions. The meta-analysis of prevalence yielded a prevalence of 0.33 (95% CI 0.11–0.60) for oral lesions in general and 0.10 (95% CI = 0.01–0.24) for aphthous lesions.
These high degrees of heterogeneity reflect the many methodological issues affecting the included studies regarding the prevalence of COVID-19 oral lesions; specific studies on the topic, with sufficient sample sizes and careful examination and classification of oral lesions, are still lacking. Any review of the topic has to rely on obtaining data from studies that either do not focus specifically on oral lesions or collect the information through patient questionnaires. Similarly, the 95% confidence intervals (disproportionately wide) of the two meta-analyses give an idea of the imprecision of the results. Therefore, the results of the meta-analysis of these variables should be viewed with caution and only as preliminary indicators to lay the groundwork for future research. In line with these observations, the GRADE assessment found that the certainty of the evidence for these two indices is low, which means that future research is very likely to change the current estimates.
As for the prevalence of xerostomia, the heterogeneity of the studies was high (I2 = 80%). In the meta-analysis, the prevalence estimate was 0.44 (95% CI 0.36–0.52). The relatively narrow range of the 95% confidence intervals bolsters the findings. In agreement with these considerations, the GRADE evaluation suggested moderate certainty of evidence in this area.
Meta-regression analysis of prevalence studies was performed in an attempt to explore the possible sources of heterogeneity in the results of these studies. The geographical location of the study, study design, and risk of bias did not show a significant effect on the prevalence estimate for oral lesions in total or the prevalence estimate for aphthous lesions. As for xerostomia, variables of study design and risk of bias showed significant effects on the prevalence estimate (R-squared = 0.9417, p < 0.003), emphasizing the need for studies with more robust quality and study design (e.g.,: prospective studies) in the future. In general, meta-regression analysis could not amply explain the sources of heterogeneity in the prevalence studies, presumably because of the paucity of eligible studies in this area.
Funnel plots of prevalence studies demonstrate noticeable asymmetry (Figures 6–8). The asymmetry is in the scatter of small studies and is evident in all three funnel plots, but this scatter is not always right-sided, as would be expected in publication bias. Funnel plots of studies on the prevalence of oral lesions in general (Figure 6) and studies on the prevalence of aphthous lesions (Figure 8) show a right-sided asymmetry, suggesting publication bias; while the funnel plot of studies on the prevalence of xerostomia shows a pronounced asymmetry to the left. This asymmetry may have arisen from inadequate detection methods in the smaller studies. Whatever the reason for this discrepancy in the results regarding xerostomia, the underreporting of this condition in smaller studies impacts the prevalence estimate of xerostomia in COVID-19.
In summary, the SRMA of prevalence data suggests a high prevalence of xerostomia. The mechanisms of this phenomenon in COVID-19 and its possible relationship with the pathologic processes of the disease are currently under discussion (90). In a broader perspective, the relatively high frequency of xerostomia and aphthous lesions in case reports and case series of oral manifestations corroborates the assertion that these two findings occur frequently in patients with COVID-19.
In this SRMA, we have proposed a framework for classifying oral lesions seen in COVID-19 according to their putative etiologies.
Oral manifestations in COVID-19 patients are varied and of diverse etiologies. To embark upon a systematic review of the oral manifestations of COVID-19, the myriad afflictions of the mouth reported in this group of patients should be scrutinized and their possible relationship with this infection examined. In this SRMA, we have proposed a framework for classifying oral lesions seen in COVID-19 according to their putative etiologies.
Many of the oral afflictions seen in COVID-19 patients are not directly caused by SARS-CoV-2 infection and, thus, should not be classified as oral manifestations of this disease. One notable group in this category is iatrogenic complications that occur in the course of the treatment of COVID-19. This group includes lesions caused by mechanical trauma of prolonged intubation and other invasive procedures employed (28, 29). Also, drug reactions presenting in the form of oral lesions have been reported (30), which can be classified in this category.
Another group of oral lesions seen in patients with COVID-19, but not directly related to the pathologic processes of SARS-CoV-2 infection, are opportunistic co-infections that involve the oral cavity. Oral co-infections reported thus far in patients with COVID-19 include candidiasis and Herpes simplex infections (31–39). As in many other debilitating diseases, the occurrence of such opportunistic co-infections is to be expected in COVID-19.
Taste disturbance/anosmia was not addressed in the present review as it clearly surpasses the confines of the oral cavity and involves the sense of smelling. Moreover, some patients with COVID-19 present with distinctive constellations of signs and symptoms that involve several organ systems including the mouth. Notable examples of such constellations are the multisystem inflammatory syndrome and Kawasaki-like disease frequently encountered in children with COVID-19 (39–52). Toxic epidermal necrolysis (TEN) and urticaria and angioedema with mucocutaneous involvement are other examples (54, 91). The presence of oral lesions in these clinical syndromes is variable, and a considerable proportion of the patients afflicted with these syndromes do not have oral lesions. Furthermore, the clinical picture of these syndromes indicates that the underlying pathological processes are much broader than the confines of the oral cavity. Therefore, while the mouth lesions in these syndromes should be noted and described, such oral involvements are better addressed in the context of the relevant clinical syndromes rather than the oral manifestations of COVID-19.
After the above-mentioned categories are excluded, a considerable body of evidence on the oral manifestations of COVID-19 remains (7, 55–89). This category includes oral lesions and salivary gland involvement. It is highly probable that many of these manifestations are directly caused by SARS-CoV-2 infection. For all these reasons, case reports and case series related to this category are discussed in more detail here. The 35 Case report and case series papers are from various locations spanning the continents of Africa, Asia, Europe, and Americas. Brazil has the highest number of publications (seven papers). A total of 236 have been described in these papers. Of the patients, 119 are female and 113 are male. In the remaining four patients, gender has not been specified. The patients range from 9 to 88 years old and represent every age group in between. The oral lesions in the patients are highly varied, with the most reported being ulcerations in various parts of the oral cavity in 12 papers. The tongue is the most frequently afflicted part of the oral cavity, reported in 20 papers.
Oral lesions likely caused by SARS-CoV2 infection present a very heterogeneous group affecting almost the entire oral cavity. The patterns of occurrence of these manifestations are gradually emerging through case reports and other observational studies, and their probable causal relationship to SARS-CoV2 remains under study. Several groups of viruses, such as herpesviruses and human papillomaviruses, are known to cause oral lesions (11, 92), and the potential of SARS-CoV2 coronavirus to cause oral lesions should be thoroughly investigated. However, the role of coincidence, comorbidities and opportunistic co-infections in the occurrence of some of these lesions cannot be ruled out at this time.
To date, no consensus has been reached on the causal relationship between SARS-CoV2 infection and oral manifestations of COVID-19 and very few studies have focused specifically on the question of the prevalence of oral lesions in COVID-19, therefore, any decision to include a particular group of lesions in this category is, to some extent, subjective.
Numerous reviews have addressed the question of oral manifestations in patients with COVID-19 (3–8) but, in general, these studies have reviewed case reports and case series and discussed the association of SARS-CoV2 infection with these manifestations. In this sense, the present RSMA agrees with previous reviews and studies, presenting, in addition, a meta-analysis on the prevalence of oral lesions in COVID-19, which will pave the way for further studies on this pathology.
The present paper reflects certain limitations. COVID-19 is a novel and rapidly evolving disease and many of its features, including the oral manifestations associated with it, are still under investigation. As yet, no consensus has been reached regarding the nature and classification of the oral lesions in COVID-19 and their causative relationship with the diseases process. This limitation is reflected in the systematic reviews of the subject such as the present paper. Moreover, there is a marked paucity of high-quality studies on the prevalence of these oral manifestations, and this limitation affects the prevalence estimates presented in this meta-analysis. The above limitations are reflected in the heterogeneity in the results of the included studies.
Conclusions
Case reports and case series describe a relatively high frequency of xerostomia and aphthous lesions in patients with COVID-19. There is a markedly paucity of specific studies on the subject, with sufficient sample sizes and careful examination and classification of oral lesions; therefore, it is suggested that more studies of robust, prospective design are conducted on oral lesions of COVID-19, with particular attention to the classification of these lesions.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
JAr, AS, and JMA: conceptualization, formal analysis, writing original draft, and supervision. JAr: methodology. NL-V: software. JAr, AS, JMA, JAl, CR, and NL-V: validation and review and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2021.726753/full#supplementary-material
References
1. Hatmi ZN. A systematic review of systematic reviews on the COVID-19 pandemic. SN Compr Clin Med. (2021) 26:1–18. doi: 10.1007/s42399-021-00749-y
2. Suthar S, Das S, Nagpure A, Madhurantakam C, Tiwari SB, Gahlot PM, et al. Epidemiology and diagnosis, environmental resources quality and socio-economic perspectives for COVID-19 pandemic. J Environ Manag. (2021) 280:111700. doi: 10.1016/j.jenvman.2020.111700
3. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, Acevedo AC, De Luca Canto G, et al. Oral manifestations in patients with COVID-19: a living systematic review. J Dental Res. (2021) 100:141–54. doi: 10.1177/0022034520957289
4. Capocasale G, Nocini R, Faccioni P, Donadello D, Bertossi D, Albanese M, et al. How to deal with coronavirus disease 2019: A comprehensive narrative review about oral involvement of the disease. Clin Exp Dent Res. (2021) 7:101–8. doi: 10.1002/cre2.332
5. de Sousa F, Paradella TC. Considerations on oral manifestations of COVID-19. J Med Virol. (2021) 93:667–8. doi: 10.1002/jmv.26451
6. Egido-Moreno S, Valls-Roca-Umbert J, Jané-Salas E, López-López J, Estrugo-Devesa A. COVID-19 and oral lesions, short communication and review. J Clin Exp Dent. (2021). 13:e287–94. doi: 10.4317/jced.57981
7. Hocková B, Riad A, Valky J, Šulajová Z, Stebel A, Slávik R, et al. Oral complications of ICU patients with COVID-19: case-series and review of two hundred ten cases. J Clin Med. (2021) 10:581. doi: 10.3390/jcm10040581
8. Paradowska-Stolarz AM. Oral manifestations of COVID-19: brief review. Dent Med Probl. (2021) 58:123–6. doi: 10.17219/dmp/131989
9. Brandini DA, Takamiya AS, Thakkar P, Schaller S, Rahat R, Naqvi AR. Covid-19 and oral diseases: Crosstalk, synergy or association? Rev Med Virol. (2021). doi: 10.1002/rmv.2226
10. Jayasrikrupaa R, Rajesh E, Masthan KMK. Oral cues in covid 19: Primary or secondary challenge. Eur J Mol Clin Med. (2020) 7:800–4.
11. La Rosa GRM, Libra M, De Pasquale R, Ferlito S, Pedullà E. Association of viral infections with oral cavity lesions: role of SARS-CoV-2 infection. Front Med. (2020) 7:571214. doi: 10.3389/fmed.2020.571214
12. Hutton B, FerránCatalá-López F, Moher D. The PRISMA statement extension for systematic reviews incorporating network meta-analysis: PRISMA-NMA. Med Clin. (2016) 16:262–6. doi: 10.1016/j.medcli.2016.02.025
13. Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, et al. Conducting systematic reviews of association (etiology): the Joanna Briggs Institute's approach. Int J Evid Based Healthc. (2015) 13:163–9. doi: 10.1097/XEB.0000000000000064
14. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
15. Aromataris E, Munn Z eds. JBI Manual for Evidence Synthesis. JBI (2020). Available online at: https://synthesismanual.jbi.global (accessed March 25, 2021).
16. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. (2013) 67:974–8. doi: 10.1136/jech-2013-203104
17. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
18. Abubakr N, Salem ZA, Kamel AHM. Oral manifestations in mild-to-moderate cases of COVID-19 viral infection in the adult population. Dent Med Probl. (2021) 58:7–15. doi: 10.17219/dmp/130814
19. Askin O, Altunkalem RN, Altinisik DD, Uzuncakmak TK, Tursen U, Kutlubay Z, et al. Cutaneous manifestations in hospitalized patients diagnosed as COVID-19. Dermatol Therapy. (2020) 33:e13896. doi: 10.1111/dth.13896
20. Biadsee A, Biadsee A, Kassem F, Dagan O, Masarwa S, Ormianer Z. Olfactory and oral manifestations of COVID-19: sex-related symptoms-a potential pathway to early diagnosis. Otolaryngol Head Neck Surg. (2020) 163:722–8. doi: 10.1177/0194599820934380
21. Fantozzi PJ, Pampena E, Di Vanna D, Pellegrino E, Corbi D, Mammucari S, et al. Xerostomia, gustatory and olfactory dysfunctions in patients with COVID-19. Am J Otolaryngol. (2020) 41:102721. doi: 10.1016/j.amjoto.2020.102721
22. Fidan V, Koyuncu H, Akin O. Oral lesions in Covid 19 positive patients. Am J Otolaryngol. (2021) 42:102905. doi: 10.1016/j.amjoto.2021.102905
23. Gherlone EF, Polizzi E, Tet,è G, De Lorenzo R, Magnaghi C, RovereQuerini P, et al. Frequent and persistent salivary gland ectasia and oral disease after COVID-19. J Dental Res. (2021) 100:464–71. doi: 10.1177/0022034521997112
24. Khabadze Z, Sobolev K, Todua I, Mordanov O. Changes in the oral mucosa and general indicators with COVID 19 (SARS-CoV-2): a single-center descriptive study. Endodontics Today. (2020) 18:4–9. doi: 10.36377/1683-2981-2020-18-2-4-9
25. Nuno-Gonzalez A, Martin-Carrillo P, Magaletsky K, Martin Rios MD, HerranzMañas C, Artigas Almazan J, et al. Prevalence of mucocutaneous manifestations in 666 patients with COVID-19 in a field hospital in Spain: oral and palmoplantar findings. Br J Dermatol. (2021) 184:184–5. doi: 10.1111/bjd.19564
26. Rekhtman S, Tannenbaum R, Strunk A, Birabaharan M, Wright S, Grbic N, et al. Eruptions and related clinical course among 296 hospitalized adults with confirmed COVID-19. J Am Acad Dermatol. (2021) 84:946–52. doi: 10.1016/j.jaad.2020.12.046
27. Riad A, Kassem I, Stanek J, Badrah M, Klugarova J, Klugar M. Aphthous stomatitis in COVID-19 patients: Case-series and literature review. Dermatol Therapy. (2021) 34:e14735. doi: 10.1111/dth.14735
28. Ramires M, Mattia MB, Tateno RY, Palma LF, Campos L.A. Combination of phototherapy modalities for extensive lip lesions in a patient with SARS-CoV-2 infection. Photodiagn Photodyn Ther. (2021) 33:102196. doi: 10.1016/j.pdpdt.2021.102196
29. Singh C, Tay J, Shoqirat N. Skin and mucosal damage in patients diagnosed with COVID-19: a case report. J Wound Ostomy Continence Nurs. (2020) 47:435–8. doi: 10.1097/WON.0000000000000690
30. Sakaida T, Tanimoto I, Matsubara A, Nakamura M, Morita A. Unique skin manifestations of COVID-19: is drug eruption specific to COVID-19? J Dermatol Sci. (2020) 99:62–4. doi: 10.1016/j.jdermsci.2020.05.002
31. Dima M, Enatescu I, Craina M, Petre I, Iacob ER, Iacob D. First neonates with severe acute respiratory syndrome coronavirus 2 infection in Romania: three case reports. Medicine. (2020) 99:e21284. doi: 10.1097/MD.0000000000021284
32. Riad A, Gad A, Hockova B, Klugar M. Oral candidiasis in nonsevere COVID-19 patients: call for antibiotic stewardship. Oral Surg. (2020). doi: 10.1111/ors.12561
33. Salehi M, Ahmadikia K, Badali H, Khodavaisy S. Opportunistic fungal infections in the epidemic area of COVID-19: a clinical and diagnostic perspective from Iran. Mycopathologia. (2020) 185:607–11. doi: 10.1007/s11046-020-00472-7
34. Salehi M, Ahmadikia K, Mahmoudi S, Kalantari S, Jamalimoghadamsiahkali S, Izadi A, et al. Oropharyngeal candidiasis in hospitalised COVID-19 patients from Iran: species identification and antifungal susceptibility pattern. Mycoses. (2020) 63:771–8. doi: 10.1111/myc.13137
35. EghbaliZarch R, Hosseinzadeh P. COVID-19 from the perspective of dentists: a case report and brief review of more than 170 cases. Dermatol Therapy. (2020) 34:e14717. doi: 10.1111/dth.14717
36. Hedou M, Carsuzaa F, Chary E, Hainaut E, Cazenave-Roblot F, Masson Regnault M. Comment on 'Cutaneous manifestations in COVID-19: a first perspective' by Recalcati S. J Eur Acad Dermatol Venereol. (2020) 34:e299–300. doi: 10.1111/jdv.16519
37. Kämmerer T, Walch J, Flaig M, French LE. COVID-19-associated herpetic gingivostomatitis. Clin Exp Dermatol. (2021) 46:174–6. doi: 10.1111/ced.14402
38. Kitakawa D, Oliveira FE, Neves de Castro P, Carvalho L. Short report - Herpes simplex lesion in the lip semimucosa in a COVID-19 patient. Eur Rev Med Pharmacol Sci. (2020) 24:9151–3. doi: 10.26355/eurrev_202009_22863
39. Roussel A, Germanaud D, Bouchoucha Y, Ouldali N, Vedrenne-Cloquet M, Castelle M, et al. Cranial polyneuropathy as the first manifestation of a severe COVID-19 in a child. Pediatr Blood Cancer. (2021) 68:e28707. doi: 10.1002/pbc.28707
40. Baradaran A, Malek A, Moazzen N, Abbasi Shaye Z. COVID-19 associated multisystem inflammatory syndrome: a systematic review and meta-analysis. Iran J Allergy Asthma Immunol. (2020) 19:570–88. doi: 10.18502/ijaai.v19i6.4927
41. Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, et al. Cardiac MRI in children with multisystem inflammatory syndrome associated with COVID-19. Radiology. (2020) 297:E283–8. doi: 10.1148/radiol.2020202288
42. Cant A, Bhujel N, Harrison M. Oral ulceration as presenting feature of paediatric inflammatory multisystem syndrome associated with COVID-19. Br J Oral Maxillofac Surg. (2020) 58:1058–9. doi: 10.1016/j.bjoms.2020.06.037
43. Chiotos K, Bassiri H, Behrens EM, Blatz AM, Chang J, Diorio C, et al. Multisystem inflammatory syndrome in children during the coronavirus 2019 pandemic: a case series. J Pediatric Infect Dis Soc. (2020) 9:393–8. doi: 10.1093/jpids/piaa069
44. Christian NA, Wadhawan J, Abdelmalek S, Pierre L, Adeyinka A. COVID-19 infection presenting with cheilitis and fever in a toddler. Cureus. (2021) 13:e12444. doi: 10.7759/cureus.12444
45. Grimaud M, Starck J, Levy M, Marais C, Chareyre J, Khraiche D, et al. Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children. Ann Intensive Care. (2020) 10:69. doi: 10.1186/s13613-020-00690-8
46. Halepas S, Lee KC, Myers A, Yoon RK, Chung W, Peters SM. Oral manifestations of COVID-2019-related multisystem inflammatory syndrome in children: a review of 47 pediatric patients. J Am Dent Assoc. (2021) 152:202–8. doi: 10.1016/j.adaj.2020.11.014
47. Labé P, Ly A, Sin C, Nasser M, Chapelon-Fromont E, Ben Saïd P, et al. Erythema multiforme and Kawasaki disease associated with COVID-19 infection in children. J Eur Acad Dermatol Venereol. (2020) 34:e539–41. doi: 10.1111/jdv.16666
48. Rekhtman S, Tannenbaum R, Strunk A, Birabaharan M, Wright S, Garg A. Mucocutaneous disease and related clinical characteristics in hospitalized children and adolescents with COVID-19 and multisystem inflammatory syndrome in children. J Am Acad Dermatol. (2021) 84:408–14. doi: 10.1016/j.jaad.2020.10.060
49. Rivera-Figueroa EI, Santos R, Simpson S, Garg P. Incomplete Kawasaki Disease in a child with Covid-19. Indian Pediatr. (2020) 57:680–1. doi: 10.1007/s13312-020-1900-0
50. Shaigany S, Gnirke M, Guttmann A, Chong H, Meehan S, Raabe V, et al. An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19. Lancet. (2020) 396:e8–10. doi: 10.1016/S0140-6736(20)31526-9
51. Verdoni L, Mazza A, Gervasoni A, Martelli L, Ruggeri M, Ciuffreda M, et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. (2020) 395:1771–8. doi: 10.1016/S0140-6736(20)31103-X
52. Young TK, Shaw KS, Shah JK, Noor A, Alperin RA, Ratner AJ, et al. Mucocutaneous manifestations of multisystem inflammatory syndrome in children during the COVID-19 pandemic. JAMA Dermatol. (2021) 157:207–12. doi: 10.1001/jamadermatol.2020.4779
53. Mazzotta F, Troccoli T, Caselli D, Bonifazi E. Acral rash in a child with COVID-19. Eur J Pediatr Dermatol. (2020) 30:79–82. doi: 10.26326/2281-9649.30.2.2104
54. Hassan K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID-19) infection. BMJ Case Rep. (2020) 13:e236981. doi: 10.1136/bcr-2020-236981
55. Afsal AS, Musthafa N, Fathima MS, Lakshmi GG. Inflammation of papillae of Wharton's duct in COVID-19 patients: a debatable entity. Spec Care Dentist. (2021) 41:127–8. doi: 10.1111/scd.12526
56. Aghazadeh N, Homayouni M, Sartori-Valinotti JC. Oral vesicles and acral erythema: report of a cutaneous manifestation of COVID-19. Int J Dermatol. (2020) 59:1153–4. doi: 10.1111/ijd.15047
57. Al-Khanati NM, Riad A, Sahloul ME, Klugar M. Aphthous-like stomatitis of COVID-19 patients: case report and review of evidence. Braz J Oral Sci. (2020) 19:1–4. doi: 10.20396/bjos.v19i0.8661354
58. Amorim Dos Santos J, Normando AGC, Carvalho da Silva RL, De Paula RM, Cembranel AC, Santos-Silva AR, et al. Oral mucosal lesions in a COVID-19 patient: new signs or secondary manifestations? Int J Infect Dis. (2020) 97:326–8. doi: 10.1016/j.ijid.2020.06.012
59. Ansari R, Gheitani M, Heidari F, Heidari F. Oral cavity lesions as a manifestation of the novel virus (COVID-19). Oral Dis. (2021) 27:771–2. doi: 10.1111/odi.13465
60. Bezerra TM, Feitosa SG, Carneiro DTO, Costa FWG, Pires FR, Pereira KMA. Oral lesions in COVID-19 infection: Is long-term follow-up important in the affected patients? Oral Dis. (2020). doi: 10.1111/odi.13705
61. Brandão TB, Gueiros LA, Melo TS, Prado-Ribeiro AC, Nesrallah A, Prado G, et al. Oral lesions in patients with SARS-CoV-2 infection: could the oral cavity be a target organ? Oral Surg Oral Med Oral Pathol Oral Radiol. (2021) 131:e45–51. doi: 10.1016/j.oooo.2020.07.014
62. CebeciKahraman F, Çaşkurlu H. Mucosal involvement in a COVID-19-positive patient: a case report. Dermatol Therapy. (2020) 33:e13797. doi: 10.1111/dth.13797
63. Chaux-Bodard AG, Deneuve S, Desoutter A. Oral manifestation of Covid-19 as an inaugural symptom? J Oral Med Oral Surg. (2020) 26:18. doi: 10.1051/mbcb/2020011
64. Ciccarese G, Drago F, Boatti M, Porro A, Muzic SI, Parodi A. Oral erosions and petechiae during SARS-CoV-2 infection. J Med Virol. (2021) 93:129–2 doi: 10.1002/jmv.26221
65. Corchuelo J, Ulloa FC. Oral manifestations in a patient with a history of asymptomatic COVID-19: case report. Int J Infect Dis. (2020) 100:154–7. doi: 10.1016/j.ijid.2020.08.071
66. Cruz Tapia RO, Peraza Labrador AJ, Guimaraes DM, Matos Valdez LH. Oral mucosal lesions in patients with SARS-CoV-2 infection. Report of four cases. Are they a true sign of COVID-19 disease? Spec Care Dentist. (2020) 40:555–60. doi: 10.1111/scd.12520
67. Díaz Rodríguez M, Jimenez Romera A, Villarroel M. Oral manifestations associated with COVID-19. Oral Dis. (2020). doi: 10.1111/odi.13555
68. Dominguez-Santas M, Diaz-Guimaraens B, Fernandez-Nieto D, Jimenez-Cauhe J, Ortega-Quijano D, Suarez-Valle A. Minor aphthae associated with SARS-CoV-2 infection. Int J Dermatol. (2020) 59:1022–3. doi: 10.1111/ijd.15004
69. Favia G, Tempesta A, Barile G, Brienza N, Capodiferro S, Vestito MC, et al. Covid-19 symptomatic patients with oral lesions: clinical and histopathological study on 123 cases of the University Hospital Policlinic of Bari with a Purpose of a New Classification. J Clin Med. (2021) 10:757. doi: 10.3390/jcm10040757
70. Glavina A, Biočina-Lukenda D, Mravak-Stipetić M, Markeljević J. Oral symptoms and lesions in SARS-CoV-2-positive patient. Oral Dis. (2020). doi: 10.1111/odi.13596
71. Indu S. Multiple oral ulcerations - An initial manifestation of COVID 19 infection: a personal experience!! J Oral Maxillofac Pathol.(2020) 24:227–9. doi: 10.4103/jomfp.JOMFP_324_20
72. Jimenez-Cauhe J, Ortega-Quijano D, Carretero-Barrio I, Suarez-Valle A, Saceda-Corralo D, Moreno-Garcia Del Real C, et al. Erythema multiforme-like eruption in patients with COVID-19 infection: clinical and histological findings. Clin Exp Dermatol. (2020) 45:892–5. doi: 10.1111/ced.14281
73. Malih N, Hajinasrollah G, Zare M, Taheri M. Unexpected presentation of COVID-19 in a 38-year-old male patient: a case report. Case Rep Dermatol. (2020) 12:124–31. doi: 10.1159/000509994
74. Martín Carreras-Presas C, Amaro Sánchez J, López-Sánchez AF, Jané-Salas E, Somacarrera Pérez ML. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis. (2021) 27:710–2. doi: 10.1111/odi.13382
75. Pangti R, Gupta S, Nischal N, Trikha A. Recognizable vascular skin manifestations of SARS-CoV-2 (COVID-19) infection are uncommon in patients with darker skin phototypes. Clin Exp Dermatol. (2021) 46:180–2. doi: 10.1111/ced.14421
76. Patel J, Woolley J. Necrotizing periodontal disease: oral manifestation of COVID-19. Oral Dis. (2021) 27:768–9. doi: 10.1111/odi.13462
77. Putra BE, Adiarto S, Dewayanti SR, Juzar DA. Viral exanthem with “Spins and needles sensation” on extremities of a COVID-19 patient: a self-reported case from an Indonesian medical frontliner. Int J Infect Dis. (2020) 96:355–8. doi: 10.1016/j.ijid.2020.05.020
78. Riad A, Kassem I, Badrah M, Klugar M. The manifestation of oral mucositis in COVID-19 patients: a case-series. Dermatol Therapy. (2020) 33:e14479. doi: 10.1111/dth.14479
79. Riad A, Kassem I, Hockova B, Badrah M, Klugar M. Tongue ulcers associated with SARS-CoV-2 infection: A case series. Oral Dis. (2020). doi: 10.1111/odi.13635
80. Riad A, Kassem I, Issa J, Badrah M, Klugar M. Angular cheilitis of COVID-19 patients: A case-series and literature review. Oral Dis. (2020). doi: 10.1111/odi.13675
81. Sinadinos A, Shelswell J. Oral ulceration and blistering in patients with COVID-19. Evid Based Dent. (2020) 21:49. doi: 10.1038/s41432-020-0100-z
82. Soares CD, de Carvalho RA, de Carvalho KA, de Carvalho MGF, de Almeida OP. Letter to editor: Oral lesions in a patient with COVID-19. Med Oral Patol Oral Cirugia Bucal. (2020 25:e563–4. 24044. doi: 10.4317/medoral.24044
83. Soares CD, Mosqueda-Taylor A, de Carvalho MGF, de Almeida OP. Oral vesiculobullous lesions as an early sign of COVID-19: immunohistochemical detection of SARS-CoV-2 spike protein. Br J Dermatol. (2021) 184:e6. doi: 10.1111/bjd.19569
84. Taşlidere B, Mehmetaj L, Özcan AB, Gülen B.Taşlidere N. Melkersson-Rosenthal syndrome induced by COVID-19: a case report. Am J Emerg Med. (2020) 41:262.e5–e7. doi: 10.1016/j.ajem.2020.08.018
85. Tomo S, Miyahara GI, Simonato LE. Oral mucositis in a SARS-CoV-2-infected patient: Secondary or truly associated condition? Oral Dis. (2020). doi: 10.1111/odi.13570
86. Capaccio P, Pignataro L, Corbellino M, Popescu-Dutruit S, Torretta S. Acute parotitis: a possible precocious clinical manifestation of SARS-CoV-2 infection? Otolaryngol Head Neck Surg. (2020) 163:182–3. doi: 10.1177/0194599820926992
87. Chern A, Famuyide AO, Moonis G, Lalwani AK. Sialadenitis: a possible early manifestation of COVID-19. Laryngoscope. (2020) 130:2595–7. doi: 10.1002/lary.29083
88. Fisher J, Monette DL, Patel KR, Kelley BP, Kennedy M. COVID-19 associated parotitis. Am J Emerg Med. (2021) 39:254.e1–e3. doi: 10.1016/j.ajem.2020.06.059
89. Lechien JR, Chetrit A, Chekkoury-Idrissi Y, Distinguin L, Circiu M, Saussez S, et al. Parotitis-like symptoms associated with COVID-19, France, March-April 2020. Emerg Infect Dis. (2020) 26:2270–1. doi: 10.3201/eid2609.202059
90. Saniasiaya J. Xerostomia COVID-19: unleashing Pandora's box. Ear Nose Throat J. (2021) 100:139S. doi: 10.1177/0145561320960353
91. Saha M, D'Cruz A, Paul N, Healy R, Collins D, Charles DA, et al. Toxic epidermal necrolysis and co-existent SARS-CoV-2 (COVID-19) treated with intravenous immunoglobulin: 'Killing 2 birds with one stone'. J Eur Acad Dermatol Venereol. (2021) 35:e97–8. doi: 10.1111/jdv.16887
Keywords: oral manifestations, oral pathology, oral diseases, COVID-19, SARS-CoV-2, systematic review, meta-analysis
Citation: Aragoneses J, Suárez A, Algar J, Rodríguez C, López-Valverde N and Aragoneses JM (2021) Oral Manifestations of COVID-19: Updated Systematic Review With Meta-Analysis. Front. Med. 8:726753. doi: 10.3389/fmed.2021.726753
Received: 18 June 2021; Accepted: 04 August 2021;
Published: 25 August 2021.
Edited by:
Yousef Saleh Khader, Jordan University of Science and Technology, JordanReviewed by:
Andree Kurniawan, University of Pelita Harapan, IndonesiaXiangyi Kong, Chinese Academy of Medical Sciences and Peking Union Medical College, China
Copyright © 2021 Aragoneses, Suárez, Algar, Rodríguez, López-Valverde and Aragoneses. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ana Suárez, ana.suarez@universidadeuropea.es
 Javier Aragoneses
Javier Aragoneses Ana Suárez
Ana Suárez Juan Algar
Juan Algar Cinthia Rodríguez4
Cinthia Rodríguez4  Nansi López-Valverde
Nansi López-Valverde Juan Manuel Aragoneses
Juan Manuel Aragoneses