Young Blood: meet the Irish doctors with a new weapon against cancer
The big read: Two committed Irish doctors are pioneering a groundbreaking new cancer treatment. They tell Fiona Ness about the perks and pain of the world of clinical trials

'I don't see many people with this," said Ivor Yeoman's doctor when the long-distance lorry driver presented at his local hospital in Shrewsbury back in August 2017.
Perfunctory blood tests had precipitated Yeoman's emergency referral after he had contacted his GP, green and shaking and complaining of a "little cough" that disappeared each morning as soon as he'd had his last spoonful of breakfast.
In his 50s, with never a sick day in his life, Yeoman was diagnosed with a rare form of aggressive blood cancer which affects less than 1,000 people in Britain and Ireland.
That was Tuesday.
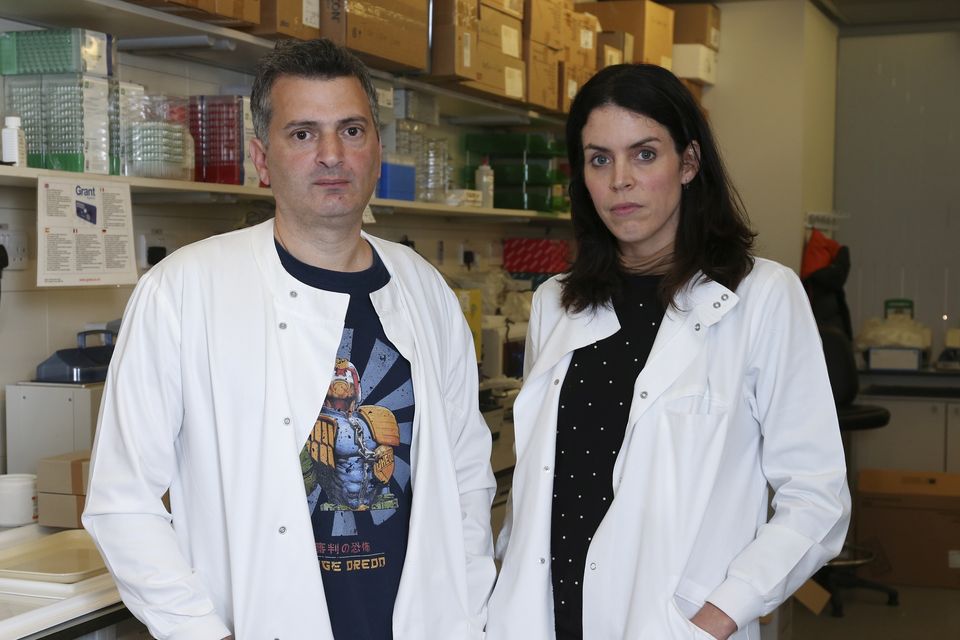
Dr Martin Pule and Dr Claire Roddie of UCL Cancer Institute in London. Photo by Gerry McManus
On Wednesday, Yeoman began six months of intense chemotherapy before undergoing a bone marrow transplant. It didn't work. The chemo was demolishing his body. He was on his last line of defence - a series of blood transfusions - and its usefulness was petering out.
"I knew then my options were limited," Yeoman says with grim optimism.
But then, hope. A new cancer trial was starting in London under the steerage of a pioneering Irish doctor, Martin Pule. Yeoman's consultant "strongly recommended" his patient apply for it.
"Similar trials had been cancelled in America after encountering problems but they'd started up in England when a doctor got a licence to treat trial patients. And being the clever man he was - a good Lego builder, I call him - he unlocked the problem, didn't he?
Huge motivation: Dr Claire Roddie in the BBC documentary War in the Blood. Photo: Richard Ansett
"It's a gift. I'm a living example of that gift."
Eight months post-treatment, Yeoman's body is showing no sign of the disease.
"It's like I've been given a new lease of life."
The end of cancer
War in the Blood, BBC. Dr Martin Pule - (C) Minnow Films - Photographer: Richard Ansett
At University College London (UCL), Dublin-born doctor Martin Pule is pioneering a cancer therapy that has the ability to change lives worldwide.
Called CAR T-cell therapy, it is proving effective against certain blood cancers that have failed all standard forms of treatment, such as chemotherapy, radiotherapy and bone marrow transplantation. The therapy reprogrammes the immune system to recognise and kill cancer cells, providing doctors with a more potent but less toxic way of treating cancer. Pule heads up the largest CAR T programme in Europe, which is running nine clinical trials. In 2014, he also founded a start-up company, Autolus, to enable him to share his team's discoveries worldwide.
The technology has been described as the beginning of the end of cancer. As we head towards a near future where it is predicted that one in two of us will develop cancer, Pule and his team believe this to be a statement of fact.
His work is groundbreaking and potentially lifesaving, yet Pule himself is at pains to emphasise that he himself is quite ordinary. In his early 40s, he brings his kids to school and collects them three days a week ("which is nice").
Pioneers: Dr Martin Pule and Dr Claire Roddie of UCL Cancer Institute in London. Photo by Gerry McManus
When the house is asleep, he works into the small hours designing, creating and modifying T-cell therapies. It's work he feels is "really something quite magical".
"As science advances, what we do in medicine is quite extraordinary. But when you're working in it, it all becomes very practical. Fundamentally, we take building blocks and stick them together and put them into cells. These tasks seem quite basic when you're stuck in the middle of it.
"I imagine the beauty and artistry that went into creating microchips in times gone past, before the work was automated - it's as creative as a Beethoven symphony. It's just that one is more accessible and the other is buried and its beauty is only accessible to a small group of key engineers who understand it. There is art and beauty and creativity in technology and I like to think that some of the engineering we've put into cells contains that too," Pule says.
"And sometimes when you have a patient who is very well and has done well in a clinical study and you're analysing their blood, and you can still see your cells that you have engineered moving around in that person's blood, you're sort of thinking, well... I designed them."
A good Lego builder
As a child, Pule says he loved creating Lego robots, the sort of stuff toy companies offload on to kids today pre-made, but which 30 years ago Pule had to teach himself circuitry and soldering to create.
Dr Martin Pule. PIC: Gerry McManus
Pule attended St Olaf's primary school in Dublin's Balally before progressing to St Benildus college in Kilmacud. Then he opted to study medicine at University College Dublin instead of what he says was a more natural choice: mathematics. His dad is a professor of maths at the university. "I felt I should be doing something intelligent and creative that you could see being used immediately rather than being very abstract... I wanted to help people," Pule says. He tried his hand at amateur film-making and played the piano, but all that fell by the wayside as his work in haematology took over.
"At one stage I like to think I was a really well-rounded individual, but now between the lab, two kids and my wife, who's a paediatric oncologist from Amsterdam… trying to keep everything going… it's fair to say that every spare minute I have I'm working.
"I'm just the same as everyone else, trying to manage family life but luckily I'm a chronic insomniac so when everyone is in bed, I stay up through the night designing stuff. I have to do that completely on my own."
Pule is a deft storyteller. His sentences tumble over each other, soft and urgent, so that the listener can't help but be gathered up and carried along on his Milky Way of words.
Pule's students at UCL must love him. He recounts how a few of them were surprised recently, when invited to lunch at his family home, that his house contained cupboards instead of laboratory shelves. Later, he admits to having looked into converting his garage into a DNA manufacturing lab. So, not exactly ordinary after all.
Pule's UCL research team is creating therapies for two specific types of blood cancers: a childhood cancer called B-cell acute lymphoblastic leukaemia (B-ALL) and diffuse large B-cell lymphoma (DLBCL) in adults. Treatments must be handmade by a team of scientists in a manufacturing lab, and customised to each individual patient.
Pule says the therapies can result in long-lasting remissions in patients with blood cancers which have failed all standard treatments.
He believes CAR T-cell therapy could become the first, rather than the last line of defence in treating blood cancers. He says it also has the potential to be developed across more cancers, including solid tumours.
Pule says good progress is being made globally in CAR T-cell therapy for the blood cancer myeloma, and a few small studies are reporting progress in using the therapy to target solid cancers, such as the Great Ormond Street Hospital trial into neuroblastoma.
"The treatment of blood cancers is often 10 years ahead of the treatment of solid cancers, mainly because solid cancers are more complex. This also makes it more difficult to target them with CAR T-cells. With lymphoma and leukaemia there are some good treatments around already - but in solid cancers such as pancreatic cancer and metastatic lung cancer, there are no good treatments," says Pule.
"If CAR T starts working at all in those areas, it will move to front-line treatment very quickly," he adds.
War in the blood
Earlier this year, the general public got to see exactly how CAR T-cell therapy affects patients, when the work of Pule's team featured in the BBC Documentary, War in the Blood. It followed scientists at University College London and clinicians at University College Hospital London (UCLH) working together on groundbreaking 'first-in-human' immunotherapy trials. The focus of the documentary were Belfast-born consultant haematologist Dr Claire Roddie and two terminally ill leukaemia patients.
Despite the fact that both patients documented on the trial died, Pule says it's important to remember that one in two patients who undergo therapy do well. "I would have been a lot happier if the documentary had afforded a more balanced representation of our work. But from a scientific point of view, the truth is that it's often the patients who don't do well on the trial that you learn the most from."
For Roddie, losing both patients on the trial was "totally tragic".
"In haematology oncology there's a lot of joy - but there's also a lot of tragedy and silence," says Roddie, her large eyes compassionate and clear.
"It takes a certain kind of… fortitude to get through that. Compassion is so important, but so is self-preservation. You need time away to help you manage that side of the job.
"Cancer: I can easily visualise what it is. I am meeting so many people who are hearing this information from me, and for the first time. I think about how it fits within the household of the individual, how it transforms the home, the workplace, the family, financial stability… Cancer isn't just for the person but for everyone associated with them. Everyone has a very different approach to dealing with the news [they are not going to get better].
"But we do just face this in therapy. If you target one thing on a cancer cell, oftentimes they are smart enough to be able to escape that targeted agent."
Telling patients that a therapy has not worked, Roddie says, is hard. "I am trying to deal with that as a human being, but also from a scientific perspective. In cancer trials, our work is [not necessarily to save lives but] to evolve our clinical practice related to those results."
The results in a clinical trial can be a terrible outcome for the patient, but Roddie says to focus on the personal tragedy is to miss the true focus of the trial: that the findings can be evolved for other patients down the track. "And hopefully, by thinking about the results in a rational, clever way, we can prevent those things happening to others."
Pule is careful to note the great debt they owe to all who agree to come on board as trial patients. As we speak, one of his trials takes a momentous step forward into "phase 2 registration" - the precursor for being licenced for use by clinicians as a cancer treatment.
We should be an army
Claire Roddie grew up in Belfast, the daughter of a paediatrician GP and Queen's University's then dean of medicine. She says her father, who died of prostate cancer in 2011, would have been very proud of her work - "he wanted me to follow in his footsteps; I always thought I'd be an actress" - and her mum is continually intrigued by the progress of the trials.
She credits her mum as being a very strong woman, running a single-handed GP practice as Roddie was growing up. She remembers dark nights sitting with her brother in the back of her mum's car, waiting for a home visit to finish, and wonders if she hasn't inadvertently become that same strong woman.
"I'm very driven. I want to make this work. Once you feel there's hope, it's very motivating. Making the treatments better and targeting more cancers is a huge motivation for me."
Part of Roddie's responsibility is to drive a huge laboratory team and keep them focused on the end goal: bringing immune therapies to as many cancers as possible. She looks forward to a future of cancer care without "hideous chemotherapeutics and radiation therapies and chemotherapies" - the cancer treatments of today that are said to work as carpet-bombing techniques, destroying many parts of the body and patient's quality of life, along with - hopefully - the cancer.
"Hopefully we will come to the point where immunotherapy can do the hard work for us."
UCLH will next year open an eight-bed unit - the Sir Naim Dangoor Centre for Cellular Immunotherapy - in a new surgery and cancer building which Roddie says will make the transmission of therapies from lab to ward much easier for all involved.
Roddie joined Pule's research team in 2015. By that time she was also a mother of two boys. She says she never had the opportunity to be an at-home mum, and despite all the demands of her work, is focused on ensuring her children don't feel as if they are taking second place in her life.
Seeing her friends, having a beer, doing a bit of exercise, blowing off a bit of steam - the rest of her time is taken up with building resilience. "You're doing nobody any favours if you work so much you burn out and turn into a cranky, non-responsive human being".
Later, an off-hand remark gives a different perspective on her 'me time'. Roddie is early to bed but rises at 4am each day to enjoy a cup of coffee on her own, read the morning papers online and work on papers and briefs - written work she knows will not be attended to the minute she arrives at the hospital and has to give patients what they need.
"Martin and I are two people when we should probably be an army."
The therapy does not work for everyone, and side effects include brain swelling and toxicity. The most promising data to date is on leukaemia, and UCL is now looking at the effects on solid cancers, while other researchers are looking at how it works with brain cancer. There also has been early success with bone marrow cancer.
In 10 years' time, Roddie hopes that the work she is doing now will have initiated a range of new, effective treatments for cancer patients across the world. The barriers to achieving this, she says, are manpower and finance.
"It takes a lot of people to make a cancer therapy, get it to the patient, and look after that patient. We need funders to continue to support these therapies and enough of us to be able to deliver them.
"If we intervene early with smart immunotherapy treatments, I don't see why we can't be in the same place with cancer in the future as we are, say, with HIV now."
What does it take to work in this area of medicine - the dedication and fortitude and unerring belief it requires? "Being an insane Irish person is the criterion for our line of work," Roddie says, laughing. "The other CAR T-cell therapy person in London is a guy called John Maher. A nice guy. It's such a high risk area you have to be slightly mad to do it."
A 'fair and affordable price'
Until a year ago, CAR T had only been available to patients in Europe through clinical trials such as Pule's, but in September 2018, drug-maker Novartis set what it called a "fair and affordable" price for its newly-licenced CAR-T therapy Kymriah.
The drug was last month made available in Britain for up to 30 children every year with acute lymphoblastic leukaemia (ALL), according to NHS England.
At the end of September, Ireland's National Centre for Pharmacoeconomics recommended that Kymriah not be considered for reimbursement by the HSE unless cost-effectiveness can be improved relative to existing treatments.
"Impressive results have been reported in clinical trials but they are expensive with a price tag of [up to] €450,000 per patient," Dr Kieran Harkin, one of the founding members of Access to Medicines Ireland (AMI), told an Oireachtas health committee earlier this year.
AMI is challenging pharmaceutical companies on their "egregious pricing strategies" which it says places medicines out of reach of most if not all patients. The organisation references recent high-profile public debates outside and inside the Dáil over the drugs Orkambi and Spinraza and predicts this occurrence will be repeated multiple times with up-and-coming CAR T therapies.
The organisation is calling on pharma companies to reconsider their pricing strategies, "to make them truly 'fair and affordable' and prioritise patients over profits," according to its spokesperson.
A spokesperson for Novartis said it had applied to the HSE for the reimbursement of its CAR-T cell therapy, Kymriah, and that HSE decision process is under way. "Novartis hopes to be able to work in partnership with the HSE to bring this treatment to patients in Ireland," the spokesperson said.
Pule is emphatic in defence of CAR T-cell costs. "You have to look at the cost and put it all the way back into the conception of the drug. For every one drug that worked, there were 20 others that didn't. And in the end, it's taken 12 years to make the drug and satisfy all the regulations around it, and the patent runs out in eight… it's hundreds of millions of dollars. I'm very careful to defend the drug companies - within reason."
In the US, some healthcare providers have negotiated with pharmaceutical companies that they will only pay if the patient is cured.
One reason why CAR T is so expensive is because it's not like manufacturing a chemical for distribution; the creation of CAR T itself is inherently expensive. The therapy has to be produced for each individual from their own blood cells.
Pule likens the procedure to the creation of the first automobile back in the 1920s, when everything was handmade and expensive until automaton came along to bring the cost of production down. Until mass production drives a reduction in CAR T-cell therapy cost, Pule says societies have to make a judgment as to what is 'worth' paying for. A further problem for health services grappling to fund the therapy is that it doesn't always work.
For Pule and his team, the challenge is to improve the treatments to make them more effective and safe. This way, he says, they can be offered as first defence rather than last resort therapies, reducing the overall cost of treating a cancer patient, and avoiding the immense trauma conventional treatments inflict on patients.
Pule says he hopes that in a small number of years, his team's therapies will be available to people for use worldwide. "It's one thing to do a scientific experiment and see how something works but quite another thing to change clinical practice. But that's how the medical community works. One person takes a step forward and the others recognise it."
Brexit is just a blip
Will all this change when Britain exits the EU? After all, the UCL trials lean on EU funding and brainpower. Cocooned behind the heavily securitised doors of UCL's building in London's bohemian Fitzrovia, Pule is adamant that the impending Brexit is "just a blip".
"The scientific and medical community has always been transnational," says Pule. "In terms of scientists getting visas to move from country to country and EU funding - those things will hurt us, but the scientific community will not wall itself off. Brexit is not going to stop us."
But then, a change of heart. Perhaps he internally analyses the data, self-edits, or simply reads the wind. "Well - maybe don't put that in - 'Martin says Brexit is just a blip!'…"
How CAR T-Cell therapy works
Pule’s immunotherapy clinical trials focus on using an immune cell called a T-cell to attack cancer. Pule visualises them as tiny robots, “moving around our body on a seek and destroy mission against infected cells”.
Although an important part of our immune system. T-cells are not good at detecting cancer. This is because cancer cells come from normal cells in our body and don’t contain foreign proteins that would cause the T-cells to target them. In addition, cancer cells like to hide from the immune system.
With CAR-T cell therapy, Pule and his team take T-cells from a patient’s blood and reprogramme them to recognise the cancer cells. They do this by inserting into the cell a new piece of DNA which tells the T-cell to make a new protein called a Chimeric Antigen Receptor (CAR). This protein acts as a sensor for the T-cells to recognise cancer.
The genetically engineered cells - which can come from the patient’s own body or a donor - are returned to the patient via a drip, with the aim that they will then move around the body, seeking out and destroying cancer cells with the same vigour they would a normal infection.
Importantly, Pule says, the CAR-T cells remain vigilant in the body once their initial work is done, protecting it against relapse. This means that for a proportion of patients who go into remission, the remission seems to be lasting.
Dr Martin Pule's CAR T-cell research is supported by the National Institute for Health Research (NIHR), University College London Hospitals (UCLH), Biomedical Research Centre (BRC) and funding by several partners including the blood cancer charity Bloodwise, and the EU 7th Framework Programme
For more of the work of Martin Pule and his team see www.ucl.ac.uk/cancer/research/ucl-car-t-programme
Join the Irish Independent WhatsApp channel
Stay up to date with all the latest news